Allergic Rhinitis: Global Trends, Socioeconomic Burden, Climate Impact & Quality of Life
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Muhammad Mudassar Hassan,MD
Last updated on February 21,2026

1. Overview: Why Allergic Rhinitis Matters Today
Allergic rhinitis (AR) is more than just seasonal sneezing — it’s a chronic inflammatory allergic disorder triggered by environmental allergens such as pollens, dust mites, pet dander, and molds. Globally, it affects between 10% and 40% of the population, causing substantial health, economic, and quality‑of‑life impacts (Ellis & Linton, 2025; Savouré et al., 2022). Unlike viral infections, allergic rhinitis arises from an immune hypersensitivity reaction involving IgE antibodies that activate inflammatory processes in the nasal mucosa.
2. Top 10 Countries Most Seriously Affected
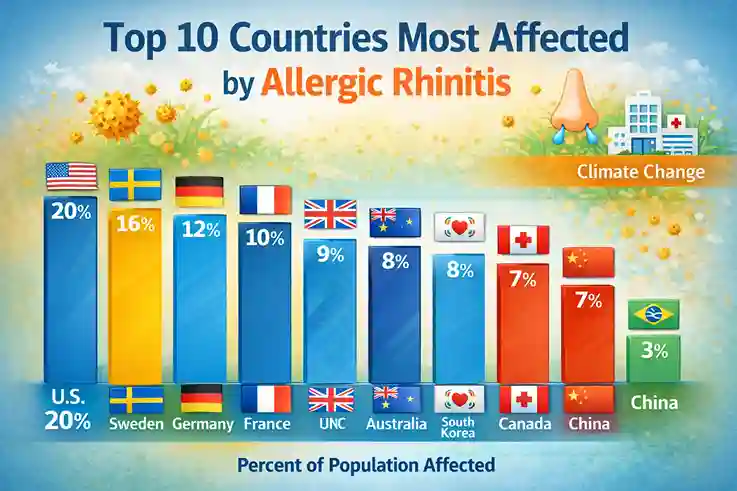
This section highlights nations reporting high disease burden, economic costs, health system impacts, or policy focus.
Rank | Country/Region |
1. United States | Large affected population and rising healthcare costs; AR care alone accounted for billions annually (Peifer et al., 2025). |
2. Sweden | National cost for AR estimated at €1.3 billion/year in a small population — marked economic burden (Bousquet et al., 2020). |
3. Germany | High prevalence and significant cost for allergic respiratory diseases in insurance data (Zhang et al., 2023). |
4. France | High seasonal allergy rates, significant workdays lost due to symptoms (Savouré et al., 2022). |
5. United Kingdom | Elevated seasonal peaks in spring and summer and higher diagnostic rates (Bousquet et al., 2020). |
6. Australia | Allergic diseases are prioritized public health concerns with documented economic impacts (Allergy.org.au, 2024). |
7. South Korea | Rapid urbanization and high prevalence of allergic diseases (Lee & Kim, 2023). |
8. China | Increasing prevalence linked to urban environments and lifestyle changes (Zhang et al., 2023). |
9. Canada | Rising health service utilization and impact on work/school productivity (Peifer et al., 2025). |
10. Brazil | High indirect cost of presenteeism and work impairment linked to AR (Imoto et al., 2024). |
3. Economic Burden & Healthcare Costs

Direct and Indirect Costs
Allergic rhinitis isn’t just about discomfort — it carries huge economic weight through direct treatment and indirect productivity losses.
- Studies estimate that in the U.S., direct treatment costs doubled over five years, exceeding $11 billion annually (Peifer et al., 2025).
- In Sweden, total costs (direct + indirect) are about €961.1 per person per year (Bousquet et al., 2020).
- Health systems in Europe face combined chronic airway disease costs (including AR) exceeding €150 billion annually (Savouré et al., 2022).
Productivity Loss
Poorly controlled AR significantly reduces workplace efficiency due to:
- Presenteeism (working while symptomatic)
- Absenteeism
- Disengagement from work tasks (Peifer et al., 2025)
One global study found that poorly controlled AR, especially when accompanied by asthma, dramatically increased work impairment (Zhang et al., 2023).
4. Policy Responses: Has the World Acted or Just Accepted It?
Public Health Recognition
Many developed nations have recognized AR within national health strategies, particularly as part of chronic respiratory disease programs.
- European countries have incorporated AR awareness within allergy and asthma frameworks and promote early diagnosis and education (Savouré et al., 2022).
- Australia has published economic impact assessments to inform policy and health spending (Allergy.org.au, 2024).
Limited Targeted Policy
Despite recognition, most countries do not have specific national policies aimed exclusively at preventing or eradicating allergic rhinitis. Rather, AR is approached as part of broader chronic respiratory disease strategies.
5. Climate Change & Allergic Rhinitis: Amplifying the Problem
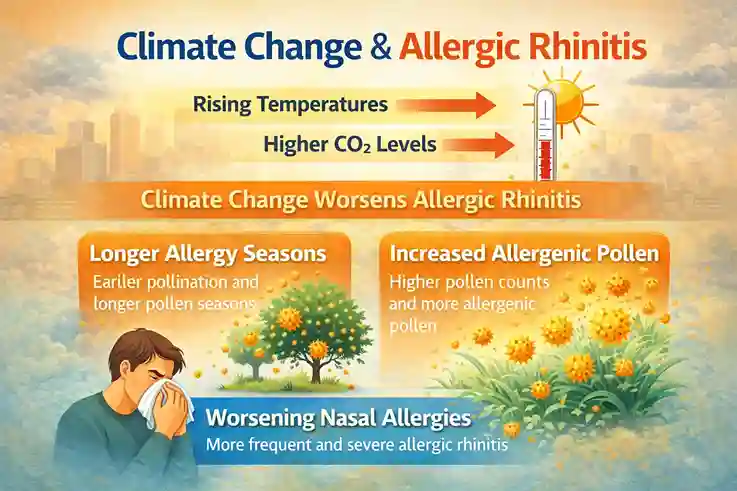
Global warming and climate change are not abstract trends — they have a direct biological and environmental impact on allergic conditions.
How Climate Affects AR
- Longer pollen seasons with higher allergen loads
- Increased airborne pollutant interaction with pollen, enhancing allergic reactions
- Greater frequency of heatwaves and wildfires, increasing respiratory stress (Savouré et al., 2022; Ziska et al., 2019)
Rising temperatures and greenhouse gas emissions amplify allergic disease risk by increasing pollen output and extending allergenic seasons (Ziska et al., 2019). These environmental changes are expected to increase both the prevalence and severity of allergic rhinitis in the coming decades, particularly in temperate regions.
6. Quality of Life & Daily Functioning: Beyond Physical Symptoms
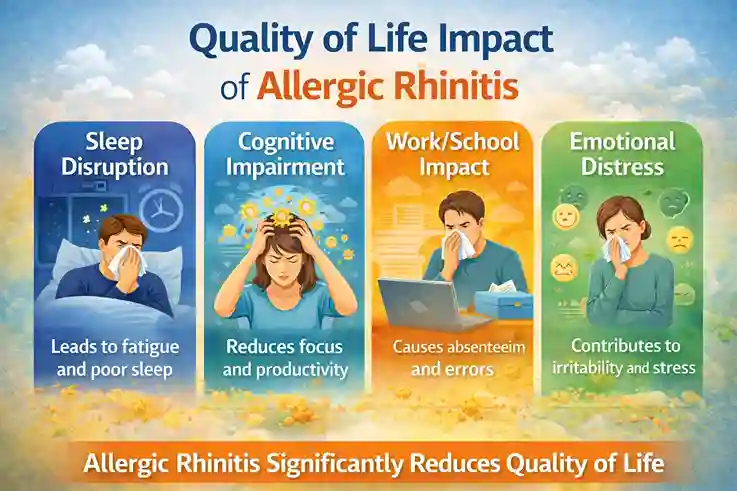
Allergic rhinitis significantly impairs quality of life across multiple dimensions:
Sleep and Daily Function
- Nasal congestion and itching can disrupt sleep cycles.
- Daytime fatigue and reduced concentration are common (Zhang et al., 2023).
Social & Behavioral Effects
- Chronic symptoms may embarrass individuals in public settings, leading to self‑consciousness or withdrawal.
- Sneezing fits in meetings, classrooms, or social gatherings can trigger stigma or anxiety, affecting confidence and self‑image (Peifer et al., 2025).
Mental Health Impact
AR symptoms often overlap with sleep deprivation, irritability, and mood disturbances. Studies link uncontrolled AR with higher rates of stress, anxiety, and diminished emotional well‑being (Zhang et al., 2023).
Behavioral Response Tips for Public Settings
- Carry tissues and use discreet nasal sprays.
- Politely excuse yourself if symptoms worsen.
- Inform close contacts you’re managing allergies to reduce social pressure.
7. Disparities: Who Suffers Most?
Socioeconomic Inequities
Low‑ and middle‑income populations often:
- Have limited access to effective treatment
- Experience higher disease burden due to environmental exposures
- Are less likely to receive immunotherapy or specialist care (Bousquet et al., 2020)
Gender & Age Differences
Although AR affects both sexes, psychosocial behavior and healthcare seeking vary:
- Adults with AR often report impaired work performance and productivity loss (Bousquet et al., 2020).
- Children may experience academic challenges and social frustration due to disrupted sleep and concentration (Imoto et al., 2024).
8. Morbidity, Mortality & Health Risks
Allergic rhinitis rarely causes death directly; mortality is extremely low, and death from AR alone is not typical. However:
- Morbidity: Chronic symptoms can exacerbate asthma and sinusitis, increasing overall health burden (Peifer et al., 2025).
- AR often coexists with asthma or chronic sinusitis, increasing disability and healthcare usage.
So while AR itself is not a leading cause of mortality, its comorbidities and chronic impacts elevate overall disease burden.
9. Strategic Budget & Resource Allocation for Future Control
Investment Needs
To reduce AR’s burden, policymakers should prioritize:
✔ Public awareness & education campaigns
✔ Improved diagnostic access
✔ Allergen avoidance strategies
✔ Subsidized treatments and immunotherapy support
✔ Research into climate‑related triggers (Savouré et al., 2022)
Current estimates show billions of USD in direct and indirect costs, suggesting targeted investments in early control may save healthcare and economic resources long‑term (Peifer et al., 2025).
10. Will Allergic Rhinitis Increase or Decrease in the Future?
The evidence points toward persistence and likely increase in allergic disease burden due to:
✔ Longer pollen seasons
✔ Urbanization and pollution
✔ Global warming
✔ Increased allergen exposure
Even if percentage prevalence stabilizes, the absolute number of affected individuals will grow with population increases and environmental changes (Ziska et al., 2019).
Conclusion
Allergic rhinitis is a global public health challenge with far‑reaching effects on economy, quality of life, mental health, and healthcare systems. While some countries have included AR within broader chronic disease policies, dedicated strategies and climate adaptation measures are urgently needed. With global environmental changes accelerating, AR is projected to become even more pervasive — making prevention, education, and equitable access to care top priorities for future health planning.
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Can allergic rhinitis be hereditary?
Yes, allergic rhinitis can run in families. Individuals with parents who have allergies are more likely to develop the condition themselves.
2. How long do allergic rhinitis symptoms last?
Symptoms can last from a few weeks to months, depending on the allergen exposure and whether it’s seasonal or perennial.
3. Can allergic rhinitis cause asthma?
Yes, allergic rhinitis is often associated with asthma, as both share similar inflammatory pathways in the respiratory system
4. Is allergic rhinitis more common in urban or rural areas?
Allergic rhinitis is more prevalent in urban areas due to higher exposure to allergens like pollution, dust, and pet dander.
5. How does air pollution affect allergic rhinitis?
Air pollution can worsen allergic rhinitis by increasing sensitivity to allergens and exacerbating symptoms, such as nasal congestion and inflammation.
6. Can allergic rhinitis cause ear problems?
Yes, untreated allergic rhinitis can lead to ear congestion and even temporary hearing loss due to fluid buildup in the middle ear.
7. What is the link between allergic rhinitis and mental health?
Persistent symptoms of allergic rhinitis can lead to stress, anxiety, and depression due to disrupted sleep and ongoing discomfort.
8. Can diet impact allergic rhinitis symptoms?
Some studies suggest that antioxidant-rich diets (e.g., fruits and vegetables) may help reduce inflammation associated with allergic rhinitis.
9. What role does immune system dysfunction play in allergic rhinitis?
In allergic rhinitis, the immune system mistakenly treats harmless substances as threats, triggering an overreaction through IgE antibodies and histamine release.
10. How effective are natural remedies for managing allergic rhinitis?
While some natural remedies like nasal irrigation and honey may provide symptom relief, they are not a substitute for medical treatments and should be used alongside conventional therapies.
References
- Bousquet, J., Schünemann, H. J., Togias, A., Zuberbier, T., Rush, N., Bachert, C., … & Haahtela, T. (2020). Allergic rhinitis. Nature Reviews Disease Primers, 6, 62. https://doi.org/10.1038/s41572-020-00227-0
- Ellis, A. K., & Linton, S. (2025). Diagnosing allergic rhinitis and local allergic rhinitis. Journal of Allergy and Clinical Immunology: In Practice, 13(12), 3456-3468.
- Peifer, S. J., Helmen, Z. M., Duffield, S., et al. (2025). The study focuses on underrepresented populations and healthcare access barriers in allergic rhinitis. The Laryngoscope, 135(9), 3071-3081.
- Savouré, M., Bousquet, J., Jaakkola, J. J. K., et al. (2022). Worldwide prevalence of rhinitis in adults: A review of definitions and temporal evolution. Clinical and Translational Allergy, 12(3), e12130. https://doi.org/10.1002/clt2.12130
- Zhang, X., Zhang, M., Sui, H., et al. (2023). Prevalence and risk factors of allergic rhinitis among Chinese adults: A nationwide representative cross-sectional study. World Allergy Organization Journal, 16(3), 100744.
- Ziska, L. H., Makra, L., Harry, S. K., et al. (2019). Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere. Science Advances, 5(7), eaav7610. https://doi.org/10.1126/sciadv.aav7610

