Best Antihistamines and Nasal Sprays for Allergic Rhinitis: A Comparison Guide
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Jamal ud Din Khan, FCPS
Last updated on February 07,2026
Choosing the right treatment for allergic rhinitis can feel overwhelming. Some medicines work quickly, others provide long-term control, and some only target specific symptoms. According to recent clinical guidance, antihistamines and nasal sprays remain the two most effective and widely used treatments for managing allergic rhinitis (Linton et al., 2023).
How Antihistamines & Nasal Sprays Work
Allergic rhinitis symptoms occur when allergens trigger histamine and other inflammatory chemicals inside the nose.
Different treatments target different parts of this reaction:
- Oral antihistamines block histamine throughout the body (Church et al., 2021).
- Intranasal antihistamines act directly in the nose and work faster (Patel et al., 2022).
- Intranasal corticosteroids (INCS) reduce nasal inflammation and remain the gold standard for congestion (Derendorf et al., 2015; Zeroli et al., 2024).
- Combination therapy (azelastine + fluticasone) offers the strongest results, especially in moderate-to-severe allergic rhinitis (Indolfi et al., 2025; Carr et al., 2012).
Understanding these differences helps you select the most effective treatment.
Oral Antihistamines
Oral antihistamines are commonly used for mild to moderate allergic rhinitis symptoms, particularly sneezing, itching, and runny nose.
First-Generation Antihistamines
Examples: Diphenhydramine, Chlorpheniramine
These medications work quickly but have strong sedation effects and short duration. Studies consistently show they impair alertness and driving performance (Linton et al., 2023). They are not recommended for daily treatment of allergic rhinitis (Scadding, 2015).
Pros
- Strong itch control
Cons
- Very sedating
- Short duration
- High side-effect burden
- Unsafe for driving
Second-Generation Antihistamines (Most Common Today)
Examples: Cetirizine, Loratadine, Fexofenadine, Desloratadine, Levocetirizine
These provide effective symptom control with minimal sedation.
Research shows they are superior for sneezing, itching, and runny nose, but still weak for nasal congestion (Torres et al., 2024).
Pros
✔ Once daily
✔ Minimal drowsiness
✔ Good symptom reduction
✔ Good safety profile
Cons
– Not ideal for congestion
– Cetirizine may cause mild sedation in a few patients
Second-generation agents are generally considered the best antihistamines for allergic rhinitis for daily symptom control because they are Non-Drowsy.
Third-Generation Antihistamines
Examples: Levocetirizine, Desloratadine
These are purified, improved forms of 2nd-generation antihistamines. Evidence shows they have lower sedation and longer duration compared to their parent molecules (Church et al., 2021).
Best for:
- People sensitive to drowsiness
- Those needing long-term daily control
- Patients who had side effects from 2nd-gen options
Comparison Table — Antihistamine Generations
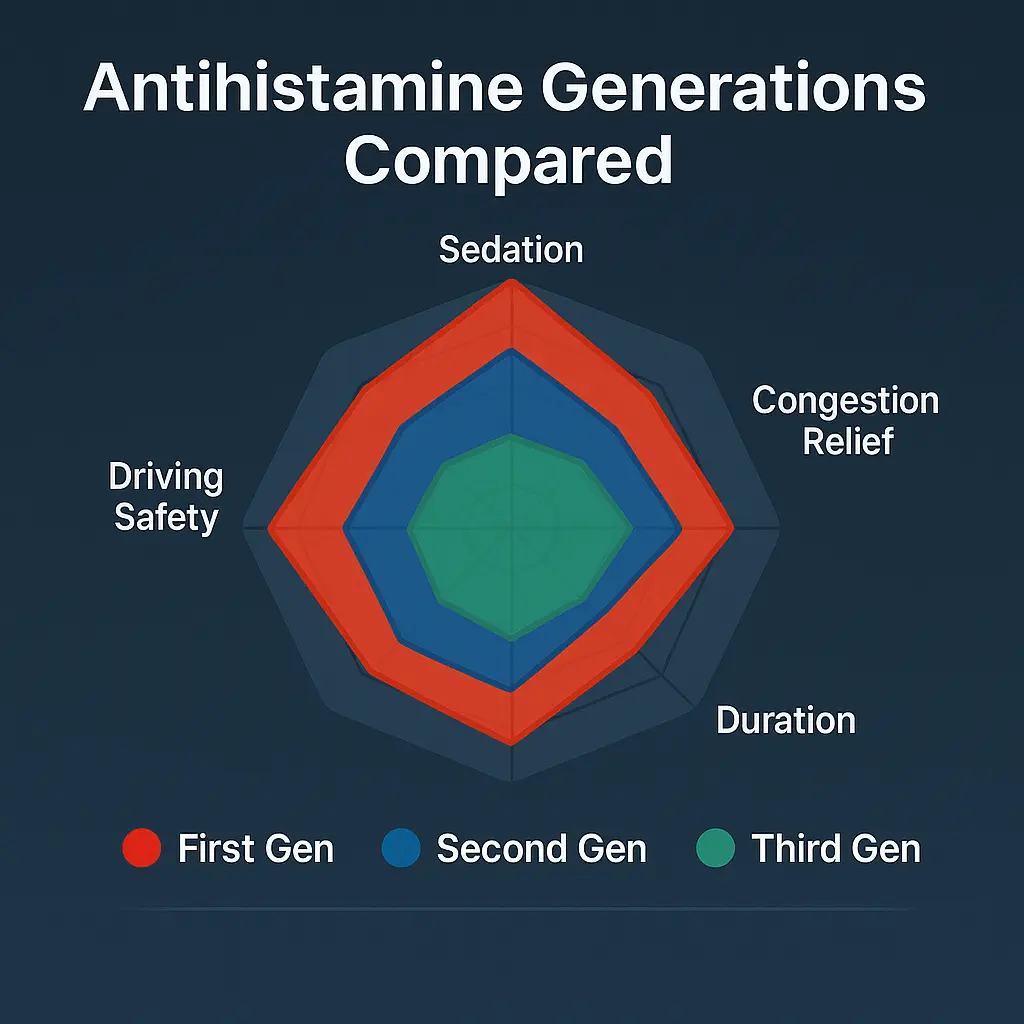
Feature | First Gen | Second Gen | Third Gen |
Sedation | Very high | Low | Very low |
Best for | Acute itch | Daily symptom control | Long-term minimal-sedation control |
Congestion relief | Poor | Poor | Poor |
Duration | Short | Long | Long |
Driving safety | Unsafe | Safe | Very safe (Linton et al., 2023) |
Intranasal Antihistamines — Fastest Symptom Relief
Examples: Azelastine, Olopatadine
Intranasal antihistamines for allergic rhinitis provide faster relief than oral agents, particularly for sneezing and rhinorrhea.
Studies show azelastine works faster than oral antihistamines and provides stronger relief for runny nose and sneezing (Meltzer et al., 2013; Patel et al., 2022).
Pros
✔ Fastest onset of action
✔ Better congestion relief than pills
✔ Can be combined with nasal steroids
Cons
– Bitter taste
– Twice-daily dosing in some cases
Intranasal Corticosteroids (INCS): Gold Standard Treatment
Examples: Fluticasone, Mometasone, Budesonide, Triamcinolone
Nasal steroid sprays for allergic rhinitis provide the strongest overall symptom control when used consistently.INCS directly reduce inflammation inside the nose. Clinical evidence shows they are the most effective treatment for congestion, post-nasal drip, and overall symptom relief (Derendorf et al., 2015; Zeroli et al., 2024).
Meta-analysis confirms nasal steroids outperform oral antihistamines in nearly every symptom category (Torres et al., 2024).
Pros
✔ Best long-term symptom control
✔ Best for nasal congestion
✔ Strong anti-inflammatory effect
✔ Excellent safety profile
Cons
– Slow onset (hours to days)
– Must be used consistently
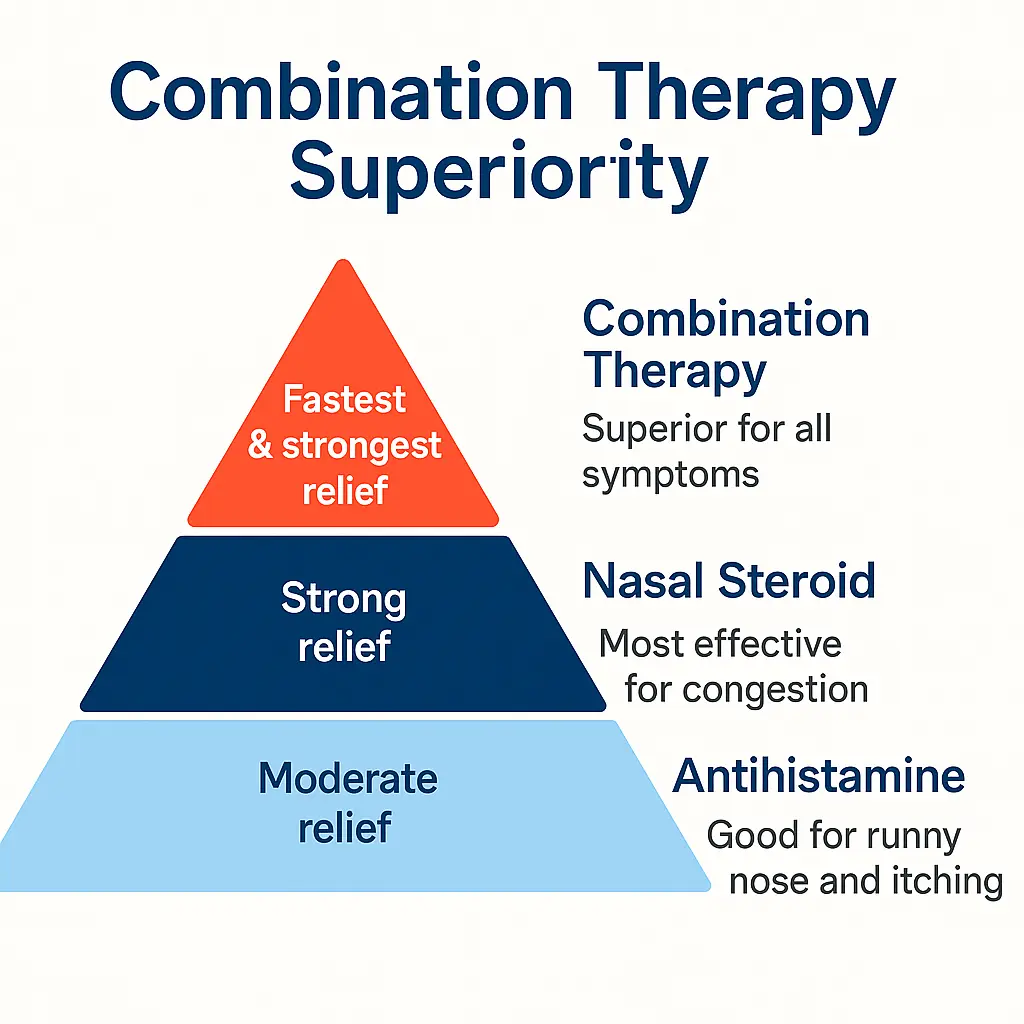
Combination Spray (Azelastine + Fluticasone)
This dual-action therapy combines:
- Azelastine → Fast antihistamine
- Fluticasone → Strong anti-inflammatory effect
Combination nasal sprays containing an antihistamine and a corticosteroid provide both rapid and sustained symptom control.
Pros
✔ Fastest AND strongest relief
✔ Best for moderate-to-severe cases
✔ Works for congestion, sneezing, itching, runny nose
Cons
– Higher cost
– Can cause mild throat irritation
This option is often referred to as a combination nasal spray for allergic rhinitis.
Nasal Steroids vs Oral Antihistamines

A 2024 systematic review found nasal steroids offer superior symptom control compared to oral antihistamines (Torres et al., 2024).
Symptom | Oral Antihistamines | Nasal Steroids |
Sneezing | Good | Excellent |
Itching | Good | Excellent |
Runny nose | Moderate | Excellent |
Congestion | Poor | Best |
Onset | ~1 hour | Hours–days |
Overall control | Moderate | Superior (Linton et al., 2023,Derendorf et al., 2015) |
If congestion is your main symptom → choose a nasal steroid.
Intranasal Antihistamines vs Intranasal Steroids
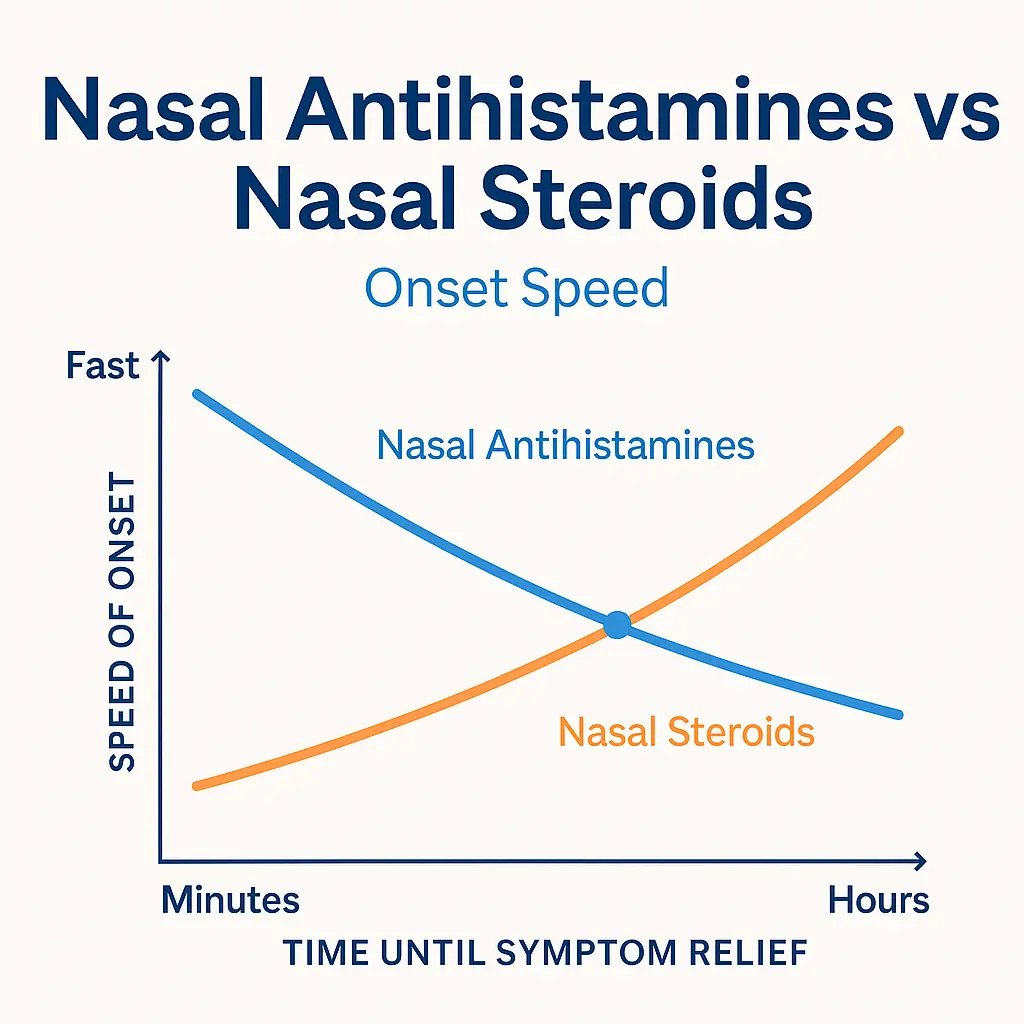
Research comparison:
Feature | Nasal Antihistamine | Nasal Steroid |
Onset | Minutes | Hours |
Strength | Moderate | Strongest |
Congestion relief | Good | Best |
Long-term control | Moderate | Excellent |
Best use | Fast relief | Daily prevention (Meltzer et al., 2013) |
Safety Comparison
Medication Type | Safety Summary |
Oral antihistamines | Very safe; sedation depends on generation (Linton et al., 2023) |
Nasal antihistamines | Safe; slight bitter taste (Patel et al., 2022) |
Nasal corticosteroids | Safe long-term; mild dryness possible (Meltzer & Wallace, 2014) |
Combination sprays | Safe; similar risks as individual components (Indolfi et al., 2025) |
Cost Summary
Treatment | Cost | Notes |
Oral antihistamines | Low | OTC, affordable |
Nasal steroids | Low–moderate | OTC/prescription |
Nasal antihistamines | Moderate | Prescription |
Combination sprays | Higher | Best overall relief |
Key Takeaways
- Oral antihistamines are good for mild symptoms but weak for congestion.
- Intranasal antihistamines work very fast.
- Intranasal steroids provide the best overall long-term control.
- Combination sprays offer the highest effectiveness across all symptoms.
- The best treatment depends on your symptoms and severity.
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. What is the best treatment for allergic rhinitis?
Nasal steroids are best for congestion, while antihistamines work well for sneezing and itching. Combination therapies offer fast, strong relief.
2. How do antihistamines work for allergic rhinitis?
Antihistamines block histamine to reduce sneezing, itching, and runny nose but aren’t as effective for congestion.
3. What’s the difference between 1st, 2nd, and 3rd-generation antihistamines?
1st-gen causes drowsiness, 2nd-gen is non-drowsy, and 3rd-gen has the least sedation with longer-lasting effects.
4. Are nasal antihistamines better than oral antihistamines?
Nasal antihistamines work faster and provide better relief for runny nose and sneezing, while oral ones take longer to act.
5. How do nasal corticosteroids work for allergic rhinitis?
Nasal steroids reduce inflammation in the nose, providing long-term relief for congestion and overall symptoms.
6. What’s the benefit of using combination therapy for allergic rhinitis?
Combination sprays give both fast and long-lasting relief, making them ideal for moderate-to-severe symptoms.
7. How quickly do nasal steroids start working?
Nasal steroids take hours to days to work but provide the best long-term symptom control.
References
Carr, W., Bernstein, J., Lieberman, P., Meltzer, E. O., Bachert, C., Price, D., O’Dowd, L., & LaForce, C. (2012). A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. Journal of Allergy and Clinical Immunology, 129(5), 1282–1289. https://doi.org/10.1016/j.jaip.2011.12.973
Church, M. K., Kolkhir, P., Metz, M., & Maurer, M. (2021). The role and mechanisms of action of antihistamines in allergic diseases. Allergy, 76(5), 1236–1248. https://doi.org/10.1111/all.14627
Derendorf, H., Meltzer, E. O., & Storms, W. W. (2015). Intranasal corticosteroids: Clinical pharmacology and therapeutic use. Allergy and Asthma Proceedings, 36(4), 268–274. https://doi.org/10.2500/aap.2015.36.3861
Indolfi, C., Klain, A., Dinardo, G., Grella, C., Di Filippo, P., Fatica, I., Napolano, V., Decimo, F., & Miraglia del Giudice, M. (2025). Azelastine–fluticasone combination therapy in allergic rhinitis: Current evidence and clinical implications in children and adults. Pharmaceuticals, 18(11), 1624. https://doi.org/10.3390/ph18111624
Linton, S., Hossenbaccus, L., & Ellis, A. K. (2023). Evidence-based use of antihistamines for treatment of allergic conditions. Annals of Allergy, Asthma & Immunology, 131(4), 412–420. https://doi.org/10.1016/j.anai.2023.07.019
Meltzer, E. O., Berkowitz, R., Grossman, J., LaForce, C., & Tantry, S. K. (2013). Comparison of azelastine nasal spray and fluticasone propionate nasal spray in the treatment of seasonal allergic rhinitis. Allergy and Asthma Proceedings, 34(1), 35–42. https://doi.org/10.2500/aap.2013.34.3633
Meltzer, E. O., & Wallace, D. (2014). Dosing and pharmacology of intranasal steroids and antihistamines. Allergy and Asthma Proceedings, 35(6), 477–485. https://doi.org/10.2500/aap.2014.35.3784
Patel, P., D’Andrea, C., & Vasquez, K. (2022). Intranasal antihistamines: Current perspectives. Journal of Asthma and Allergy, 15, 107–120. https://doi.org/10.2147/JAA.S336709
Scadding, G. K. (2015). Optimal management of allergic rhinitis. Archives of Disease in Childhood—Education & Practice Edition, 100(2), 57–63. https://doi.org/10.1136/archdischild-2013-305666
Torres, M. I., Smith, L. E., Patel, P., & Durham, S. R. (2024). Intranasal versus oral treatments for allergic rhinitis: A systematic review and meta-analysis. Journal of Allergy and Clinical Immunology: In Practice, 12(6), 1330–1344. https://doi.org/10.1016/j.jaip.2024.03.021
Zeroli, C., Gorica, A., Monti, G., Castelnuovo, P. G. M., Bignami, M., & Macchi, A. (2024). A systematic review of randomized controlled trials on topical nasal steroids. Acta Otorhinolaryngologica Italica, 44(2), 71–75. https://doi.org/10.14639/0392-100X-N2745

