Breathing Exercises for Allergic Rhinitis & Nasal Congestion
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by:Arifa Sarfaraz,DPT & Dr. Jamal Ud Din Khan,FCPS
Last updated on February 13,2026
Allergic rhinitis (hay fever) commonly causes nasal congestion, mouth breathing, sinus pressure, disturbed sleep, and reduced lung comfort. While medications such as antihistamines and nasal corticosteroids reduce inflammation, breathing patterns themselves play a major role in symptom severity and daily comfort. Evidence shows that nasal breathing, diaphragmatic breathing, and controlled respiratory exercises can improve airflow, reduce nasal resistance, calm airway irritation, and enhance overall respiratory efficiency—especially when combined with standard medical care (Bousquet et al., 2020; Courtney, 2009).
This step-by-step guide explains how to breathe correctly with allergic rhinitis, why it works, and how to safely practice breathing exercises at home.
Why Breathing Exercises Matter in Allergic Rhinitis

Allergic rhinitis causes inflammation of the nasal mucosa, leading to obstruction and a shift toward mouth breathing. Mouth breathing bypasses nasal filtration and humidification, which can:
- Worsen airway dryness
- Increase exposure to irritants
- Reduce nitric oxide delivery from the nasal passages
- Aggravate chest tightness and fatigue
Breathing exercises help by:
- Improving nasal airflow
— mechanisms supported by National Institutes of Health respiratory research.
- Reducing respiratory muscle tension
- Supporting sinus drainage
- Enhancing oxygen efficiency
- Improving sleep quality and daytime energy
These effects are supported by respiratory physiology and allergy research (Bousquet et al., 2020; Courtney, 2009).
Foundational Rule: Nasal Breathing First
Before any exercise, remember this rule:
The nose is the primary breathing organ, even during mild congestion.
Nasal breathing:
- Filters allergens and particles
- Humidifies and warms air
- Produces nitric oxide, which improves airway function and oxygen uptake
Whenever possible, perform all exercises through the nose, gently and without force.
Step-by-Step Breathing Exercises for Allergic Rhinitis
1. Diaphragmatic (Belly) Breathing
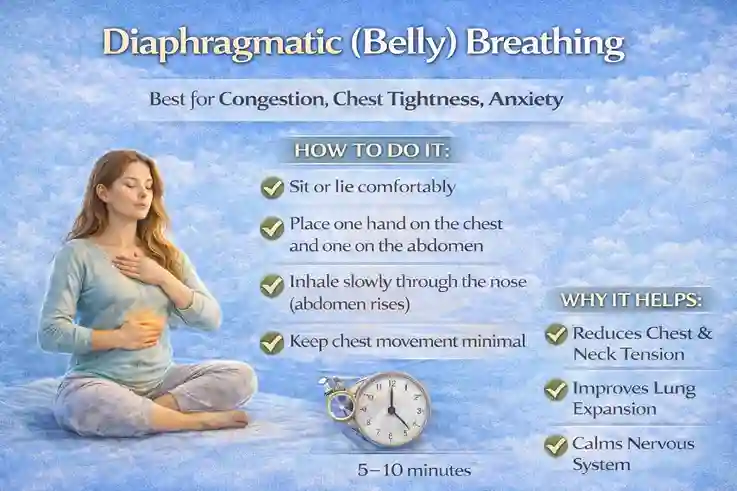
Best for: Daily congestion, chest tightness, fatigue, anxiety
How to do it:
- Sit or lie comfortably
- Place one hand on your chest, one on your abdomen
- Inhale slowly through the nose (abdomen rises)
- Keep chest movement minimal
- Exhale slowly through the nose
- Repeat for 5–10 minutes
Why it helps:
- Reduces overuse of neck and chest muscles
- Improves lung expansion
- Calms the nervous system
- Enhances oxygen efficiency
Clinical relevance: Diaphragmatic breathing improves ventilation efficiency and reduces dyspnea (Courtney, 2009).
2. Nasal Resistance Breathing (Gentle Nose Breathing)
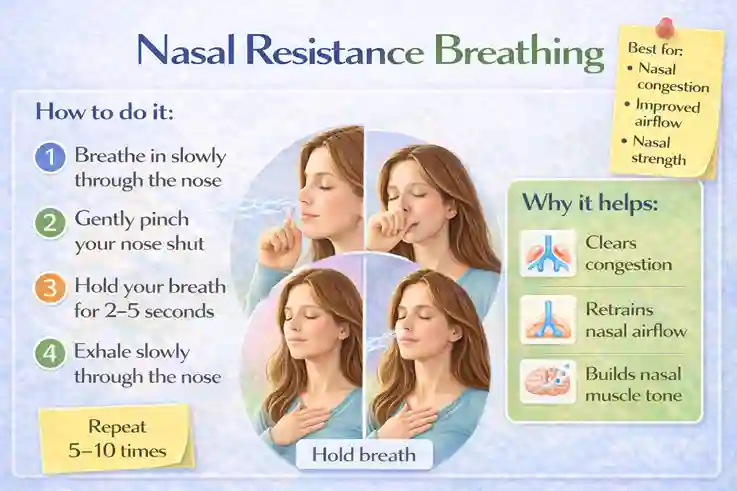
Best for:
Training nasal airflow during mild congestion
How to do it:
- Sit upright
- Breathe gently through the nose
- Reduce airflow slightly (not forcefully)
- Maintain slow, quiet breaths
- Practice for 3–5 minutes
Why it helps:
- Encourages nasal patency
- Improves tolerance to nasal breathing
- Reduces habitual mouth breathing
3. Alternate Nostril Breathing (Modified – Allergy-Safe)
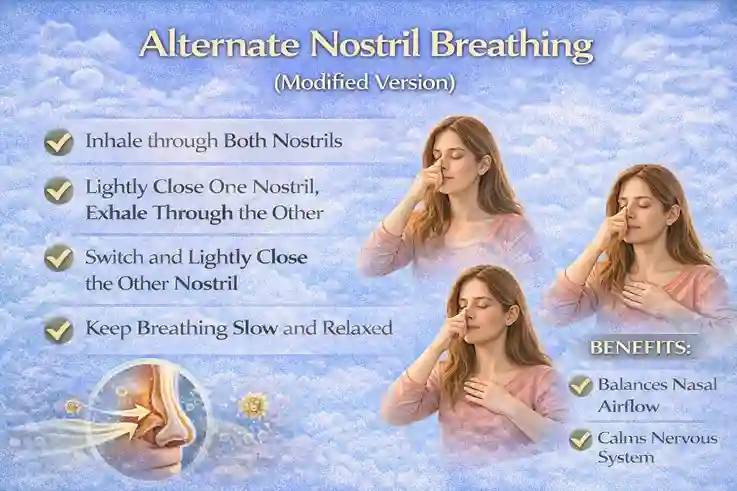
Best for:
Nasal balance, relaxation, sinus comfort
How to do it (gentle version):
- Sit comfortably
- Inhale through both nostrils
- Lightly close one nostril and exhale through the other
- Switch sides
- Keep breathing slow and relaxed
- Continue for 3–5 minutes
⚠️ Avoid forceful breath retention if congestion is severe.
Why it helps:
- Promotes nasal airflow balance
- Reduces perceived congestion
- Calms autonomic nervous system
4. Pursed-Lip Breathing
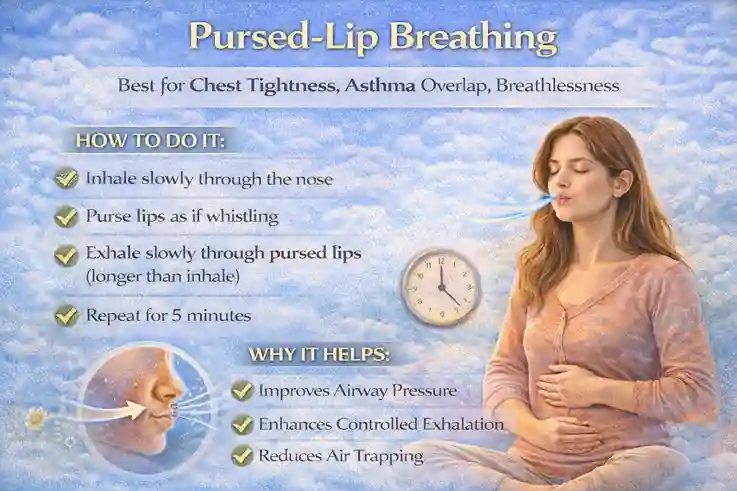
Best for:
Chest tightness, asthma overlap, breathlessness
How to do it:
- Inhale slowly through the nose
- Purse lips as if whistling
- Exhale slowly through pursed lips (longer than inhale)
- Repeat for 5 minutes
Why it helps:
- Improves airway pressure
- Enhances controlled exhalation
- Reduces air trapping
Often recommended in respiratory rehabilitation programs.
5. Morning Nasal Activation Breathing
Best for:
Morning congestion (common in allergic rhinitis)
How to do it:
- Use saline spray or rinse first as part of your daily nose & sinus care routine
- Sit upright
- Perform slow nasal inhalation
- Gentle nasal exhalation
- Add light chest expansion
- Continue for 5 minutes
This prepares nasal passages for daytime allergen exposure and fits well into a structured daily lifestyle routine to reduce allergic rhinitis naturally.
Breathing Exercises for Better Sleep With Allergic Rhinitis
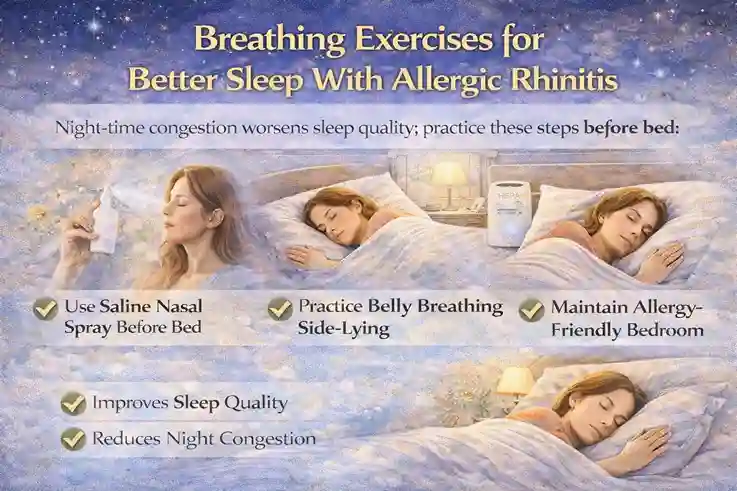
Night-time congestion worsens sleep quality— a pattern explained in why allergic rhinitis gets worse at night.
.
Before bed routine:
- Saline nasal spray
- Diaphragmatic breathing (5–10 minutes)
- Nasal breathing in side-lying or elevated head position
Studies show controlled breathing improves sleep quality and reduces nocturnal symptoms (Bousquet et al., 2020).
How Often Should You Practice?
Time | Recommendation |
Morning | 5–10 minutes |
Daytime | Short sessions if congested |
Evening | 5–10 minutes |
Before bed | Strongly recommended |
Consistency is more important than intensity.
Safety Notes (Important)
- Never force nasal breathing during severe obstruction
- Stop if dizziness occurs
- Children should be supervised
- Breathing exercises do not replace medications in moderate–severe disease— see the complete allergic rhinitis treatment guide for medical options.
When Breathing Exercises Help Most
They are especially effective when combined with:
- Saline nasal care
- Environmental control
- HEPA air purification — learn how to optimize HEPA air purification for allergy relief
- Proper medical therapy
This combined approach aligns with international allergy guidelines (Dykewicz et al., 2020).
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1.Can breathing exercises reduce nasal congestion?
Yes. They improve airflow perception and respiratory efficiency but do not replace anti-inflammatory treatment.
2.How long before I notice benefits?
Many people feel improvement within 1–2 weeks of consistent practice.
3.Are breathing exercises safe for asthma patients?
Yes, when practiced gently. Asthma patients should follow medical advice.
4.Can children do these exercises?
Yes, with age-appropriate guidance and supervision.

