Prevention of Allergic Rhinitis (Hay Fever): Practical Ways to Reduce Triggers
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Muhammad S. Anil, MD
Last updated on February 07,2026
Allergic rhinitis, commonly known as hay fever, occurs when the immune system overreacts to inhaled allergens such as pollen, dust mites, pet dander, mold spores, or cockroach particles. While allergic tendencies cannot be completely eliminated, preventive strategies can significantly reduce allergen exposure and help limit symptom severity.

Prevention strategies for allergic rhinitis focus on identifying triggers, minimizing exposure, improving indoor air quality, and using preventive medical approaches when necessary.
Know Your Allergy Triggers Before You Prevent Symptoms
Effective prevention of allergic rhinitis begins with identifying personal allergy triggers.
Common triggers of allergic rhinitis
- Tree, grass, and weed pollens
- Outdoor mold spores
Indoor allergens
- Dust mites in bedding and carpets
- Pet dander (skin flakes, saliva, fur)
- Indoor mold in damp areas
- Cockroach droppings and debris
Irritants that worsen symptoms
- Cigarette smoke and air pollution
Cleaning agents, perfumes, and industrial chemicals
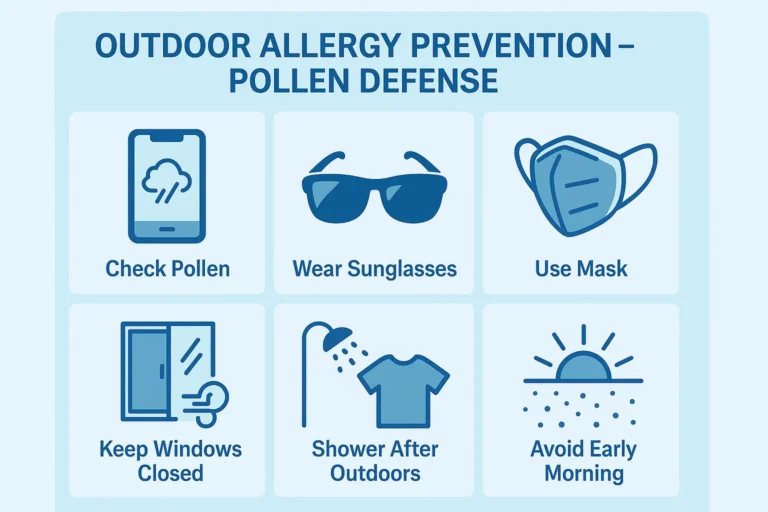
Outdoor Allergy Prevention Tips (Pollen, Spores, and Pollution)
Outdoor allergens are a primary cause of seasonal allergic rhinitis in spring, summer, and fall.
Check Pollen Count and Plan Your Day
• Check daily pollen and mold forecasts (National Allergy Bureau, weather apps, and local allergy centers).
• On high pollen days, limit outside activity, especially in the early morning.
To prevent allergies, avoid engaging in exercise near grass, fields, or freshly cut lawns.
Consult your doctor about starting allergy medications 1-2 weeks before the peak pollen season.
Protect Your Eyes, Nose, and Lungs Outside
- Wear wraparound sunglasses to reduce pollen entry in the eyes.
- Use a soft nasal barrier gel or balm inside the nostrils to trap pollens.
- Consider a well-fitting mask (N95/KN95/FFP2) on high-pollen or windy days, especially if you have asthma as well.
Stop Pollens From Coming Inside Your Home or Car
- Use air conditioning system during peak pollen hours and close the windows.
- Use recirculation mode and a cabin filter in your automobiles instead of outside air.
After spending time outside: - To remove pollen, shower and wash your hair.
- Change clothes and place them in a covered washing bin.
- Avoid drying clothes outside during high pollen seasons, since pollen can attach to fabric and increase symptoms.
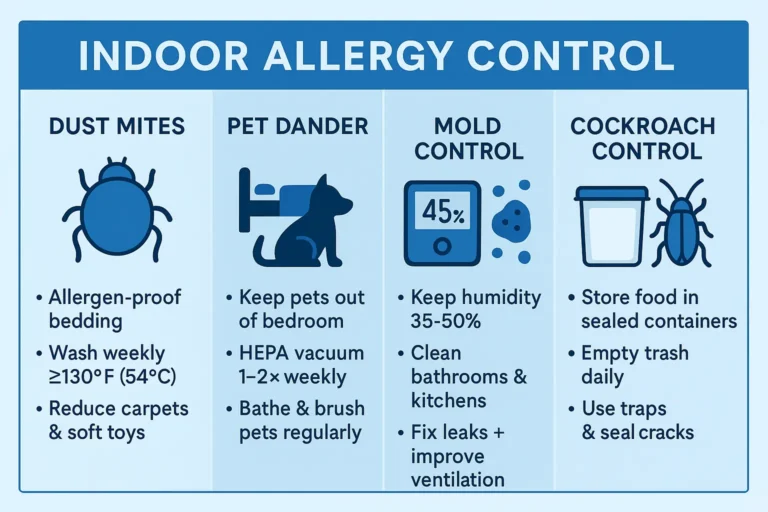
Indoor Allergy Prevention at Home (Dust Mites, Pets, Mold, Cockroaches)
Indoor allergens are the main cause of perennial allergic rhinitis.
Dust Mite Control in Bedroom and Bedding
Dust mites are one of the major causing and best-studied triggers of allergic rhinitis and asthma. Reducing exposure can significantly improve symptoms (German et al., 2002).
Key steps:
- Allergen-proof bedding
- Use mite-proof covers for mattress, pillows, and box spring.
- Close them fully with zippers.
- Wash bedding correctly
- Wash sheets, pillowcases, and blankets weekly in hot water ≥130°F (≥54°C).
- Dry on high heat if fabric allows.
- Simplify and clean the bedroom
- Remove wall-to-wall carpets where possible.
- Use low-pile, washable rugs
- Replace heavy curtains with blinds or washable shades.
- Keep soft toys to a minimum and wash them regularly.
Pet Dander Prevention in Allergy-Friendly Homes
Even “hypoallergenic” animals release dander and saliva proteins that can cause allergic rhinitis.
- Keep pets out of the bedroom and off beds/sofas.
- Ask a non-allergic person to brush and bath pets regularly (preferably outdoors or in a well-ventilated area).
- Vacuum floors and furniture with a HEPA vacuum designed for pet hair.
Mold and Moisture Control (Bathrooms, Kitchens, Basements)
Mold spores can trigger nasal congestion, sinus pressure, and asthma flares.
- Keep indoor humidity between ~35–50%; use dehumidifiers in damp areas.
- Use exhaust fans in bathrooms and kitchens when cooking or showering.
- Clean tiles, grout, and shower curtains regularly with anti-mold solutions.
- Fix leaks quickly (pipelines, roof, and basement seepage).
- Avoid storing piles of damp cardboard, newspapers, or firewood indoors.
Cockroach Allergen Control in Kitchens and Apartments
Cockroach droppings and body fragments are a known asthma and rhinitis trigger in many urban settings.
- Never leave dirty dishes overnight.
- Store food in sealed containers.
- Take trash out regularly and use bins with lids.
- Fix leaks under sinks and behind appliances.
- Use traps, gels, or professional pest control if needed.
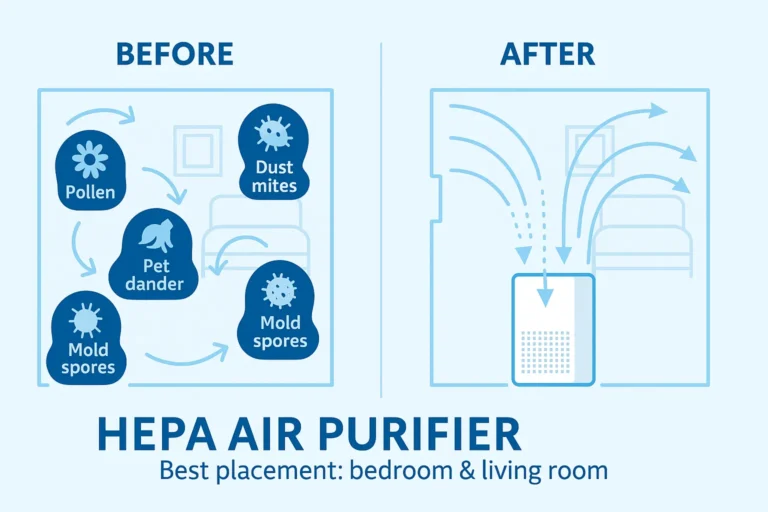
Improve Indoor Air Quality (HEPA Filters, Humidity, Ventilation)
Clean indoor air reduces exposure to multiple allergens at once.
HEPA Air Purifiers for Allergic Rhinitis Relief
Room air cleaners equipped with high-efficiency particulate air (HEPA) filters are one of the most effective ways to reduce airborne allergens such as dust mites, pet dander, mold spores, and pollen. Clinical trials show that patients with perennial allergic rhinitis and asthma experience significant symptom improvement when HEPA air cleaners are used consistently in bedrooms and high-traffic living areas (Reisman et al., 1990).
Best practices for maximum benefit:
- Place HEPA units in the bedroom and main living spaces.
- Choose a purifier with the appropriate CADR rating for your room size.
- Change HEPA filters according to manufacturer recommendations.
Vacuuming, Cleaning, and Ideal Indoor Humidity Levels
Maintaining a clean indoor environment is essential for reducing allergy triggers that collect in carpets, fabrics, and dusty corners.
- Vacuum carpets, rugs, and upholstery 1–2 times per week using a sealed HEPA vacuum.
- Dust surfaces with a damp cloth or microfiber towel to prevent allergens from circulating.
- Keep indoor humidity between 35–50%:
- Use humidifiers in dry climates.
- Use dehumidifiers in damp climates or basements.
- Clean or replace HVAC filters regularly; allergen-rated filters offer the best protection.

Lifestyle Changes to Prevent Allergy Flares
Daily lifestyle changes can make a big difference in reducing allergic rhinitis symptoms and flare-ups.
- Keep windows closed during high-pollen hours.
- Avoid cigarette smoke completely—both active and passive.
- Minimize exposure to strong air fresheners, incense, sprays, or harsh cleaning agents.
- Wear a mask and gloves when cleaning dusty areas or handling chemicals.
- Reduce clutter that attracts dust, such as extra cushions, unused fabrics, and piles of paper.
Natural & Non-Drug Strategies (Saline Rinses, Nasal Care)
Non-medication methods can gently help to reduce the allergen load inside your nose and improve breathing comfort.
- Saline nasal rinses (neti pot, squeeze bottle, or spray) flush out pollen, dust, and mucus.
- You may use isotonic or hypertonic saline depending on your clinician’s recommendation.
- Always prepare saline with distilled, boiled, or sterile water to ensure safety.
Medication-Based Prevention
Medication-based prevention plays a key role in managing allergic rhinitis symptoms, especially when complete allergen avoidance is not possible.
Intranasal Corticosteroid Sprays
- Considered as the first-line therapy for moderate to severe allergic rhinitis.
- Reduce inflammation, congestion, sneezing, and nasal swelling when used correctly and consistently (Dykewicz et al., 2020).
Oral and Intranasal Antihistamines
- Helpful for controlling itching, sneezing, watery eyes, and runny nose.
- Non-sedating, once-daily antihistamines are generally preferred.
Other possible options (under medical supervision):
- Mast cell stabilizers (e.g., cromolyn sprays) — most effective when started before allergen exposure.
- Short-term decongestant sprays — provide quick relief but should not be used long-term due to rebound congestion.
Always consult your doctor or allergist before starting, stopping, or changing any medication.
Long-Term Prevention With Allergen Immunotherapy
Allergen immunotherapy (allergy shots or sublingual tablets) trains the immune system to react less strongly to specific allergens such as pollen, dust mites, molds, or pet dander.
Benefits shown in guidelines and trials include:
- Reduced symptom severity over time.
- Lower reliance on medications.
- Long-lasting improvement even after treatment ends.
- Potential prevention of asthma progression in certain patients.
Immunotherapy is typically prescribed by an allergist after diagnostic testing identifies the most significant allergens.
Special Prevention Tips for Children, Adults, and People With Asthma
Children
- Wash soft toys weekly or freeze them overnight if washing is not possible.
- Keep pets out of children’s bedrooms.
- Avoid passive smoke completely.
Adults
- Use allergen-proof bedding and HEPA vacuum cleaners.
- Check pollen forecasts before planning outdoor activities.
- Prioritize sleep hygiene, as nasal congestion often worsens at night.
People With Asthma + Allergic Rhinitis
- Follow an asthma action plan created with your doctor.
- Use HEPA air purifiers and maintain strict dust-mite control.
- Seek regular review if you notice wheezing, chest tightness, or night cough.
Pollen Seasons in the USA: When to Start Prevention
Due to climate change and rising temperatures, pollen seasons across the United States are becoming longer and more intense (Ziska et al., 2019). Understanding seasonal changes helps you stay ahead of symptoms.
Main Outdoor Allergy Seasons in the United States
Season | Typical Months (USA) | Main Sources |
Tree pollen season | Feb – May | Oak, birch, maple, cedar, pine |
Grass pollen season | May – July | Bermuda, ryegrass, Kentucky bluegrass |
Weed pollen season (ragweed) | Aug – Nov | Ragweed, pigweed, sagebrush, lamb’s quarters |
Outdoor mold spores | Apr – Oct (year-round in warm areas) | Wet soil, leaves, compost, damp wood |
- Southern and coastal states often experience longer seasons due to milder winters.
- Northern and Midwestern regions may have shorter but more intense seasonal bursts.
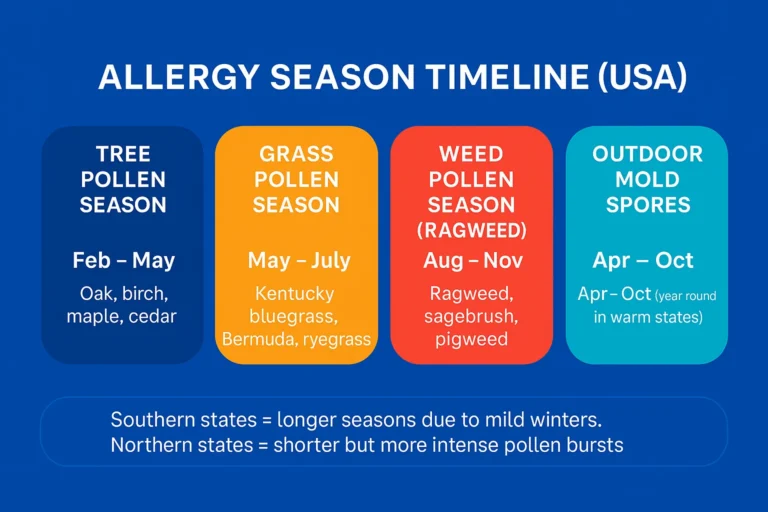
How to Use Pollen Seasons for Better Prevention
- Begin preventive medication (if prescribed) 1–2 weeks before your main allergy season starts.
- Use pollen apps and local forecasts to decide:
- When to keep windows closed.
- When to shower and change clothes after outdoor exposure.
- When to increase HEPA air purifier use indoors.
When to See an Allergist or ENT for Personalized Prevention
Consider consulting a specialist if:
- Symptoms persist for weeks or occur year-round.
- Over-the-counter treatments are not effective.
- You experience asthma symptoms, repeated sinus infections, or ear problems.
- You want to explore allergen immunotherapy.
- Your diagnosis is unclear (possible mixed rhinitis or chronic sinusitis).
A specialist can offer:
- Targeted allergy testing.
- A personalized prevention plan.
- Safe adjustments to medications.
- Guidance on long-term treatments such as immunotherapy.
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Can allergic rhinitis be completely prevented?
No. You cannot fully “prevent” the allergy tendency, but you can greatly reduce symptoms by avoiding triggers, improving air quality, and using medicines correctly.
2. What is the best way to prevent dust mite allergy symptoms?
Use mite-proof mattress and pillow covers, wash bedding weekly in hot water, keep humidity under 50%, and vacuum with a HEPA vacuum.
3. How can I reduce pollen exposure during allergy season?
Check pollen forecasts, keep windows closed, shower and change clothes after being outdoors, use HEPA air purifiers, and wear masks and sunglasses outside.
4. Do air purifiers really help with allergic rhinitis?
Yes. HEPA air purifiers reduce airborne allergens and have shown measurable symptom improvement in clinical studies (Reisman et al., 1990).
5. Are natural options like saline rinses enough to manage symptoms?
Saline rinses help clear pollen and mucus, but moderate to severe allergies often require medication or immunotherapy.
6. When should I start seasonal allergy medications?
Experts often recommend starting them 1–2 weeks before allergy season begins, but always follow your doctor’s guidance.
7. Do lifestyle habits truly matter?
Yes. Simple habits like closing windows, avoiding smoke, washing bedding, using HEPA filters, and cleaning regularly can significantly reduce the intensity and frequency of allergy flares.
References
Dykewicz, M. S., Wallace, D. V., Baroody, F., Bernstein, J., Craig, T., Finegold, I., … Portnoy, J. (2020). Rhinitis 2020: A practice parameter update. Journal of Allergy and Clinical Immunology, 146(4), 721–767.
Reisman, R. E., Mauriello, P. M., Davis, G. B., Georgitis, J. W., & DeMasi, J. M. (1990). A double-blind study of the effectiveness of a high-efficiency particulate air (HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. Journal of Allergy and Clinical Immunology, 85(6), 1050–1057.
Ziska, L. H., Makra, L., Harry, S. K., Bruffaerts, N., Hendrickx, M., Coates, F., … Knowlton, K. (2019). Temperature-related changes in airborne allergenic pollen abundance and seasonality across the Northern Hemisphere: A retrospective data analysis. The Lancet Planetary Health, 3(3), e124–e131.
American College of Allergy, Asthma & Immunology. (n.d.). Hay fever (rhinitis): Symptoms, diagnosis, management & treatment. Retrieved 2025, from the ACAAI public website.
Cleveland Clinic. (n.d.). Allergic rhinitis (hay fever): Symptoms & treatment. Retrieved 2025, from Cleveland Clinic Health Library.

