Steroids, Special Situations, and Differential Diagnosis in Allergic Rhinitis
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Muhammad S. Anil, MD
Last updated on February 08,2026
While most patients with allergic rhinitis respond to standard therapies, a subset may require advanced or specialized management. This includes short-term systemic steroids, biologic therapies in selected cases, and tailored approaches for children, pregnancy, and patients with asthma. Accurate differentiation between allergic rhinitis and viral infections is also essential for appropriate care.
This guide explains exactly when these treatments are used, their benefits, risks, and how to distinguish allergic rhinitis from the common cold, a confusion many people face.
Oral & Injectable Steroids for Allergic Rhinitis

Patients mostly ask that are oral steroids safe for allergic rhinitis? According to research, systemic steroids whether taken orally or injected are powerful anti-inflammatory medications. However, experts agree they should be used only for very short durations in severe, uncontrolled allergic rhinitis, due to potential side effects (Klimek et al., 2024).
When Are Systemic Steroids Used?
Doctors consider short courses of oral steroids ONLY when:
- Severe nasal obstruction
- Strong inflammation unresponsive to sprays
- Severe flare before an important event
- Nasal polyps with allergy
- Before or during immunotherapy initiation (in selected cases)
They are not recommended for routine or long-term allergy management (Dykewicz et al., 2020).
Oral Steroids
✔ Benefits
- Fast relief (24–48 hours)
- Improves severe congestion
- Helps when other treatments fail
❌ Risks (especially if repeated)
- Increased blood sugar
- Mood changes
- Weight gain
- Fluid retention
- Weakening of bones
- Suppressed immune response
- Adrenal suppression
👉 Because of these risks, repeated oral steroid courses are discouraged.
These medications are commonly referred to as oral steroids for allergic rhinitis when administered systemically.
Injectable Steroids (Depot Steroids)
Some clinics offer long-acting steroid injections, but modern guidelines advise against them because they remain in the body for weeks and cause unpredictable side effects, including:
- Adrenal suppression
- High blood sugar
- Bone loss
- Cataracts
ARIA and AAAAI guidelines strongly warn against routine use (Bousquet et al., 2020).
👉 Injectable steroids should be avoided unless absolutely necessary. Current guidelines advise against routine use of injectable steroids for allergic rhinitis.
Biologics for Allergic Rhinitis and Asthma Overlap
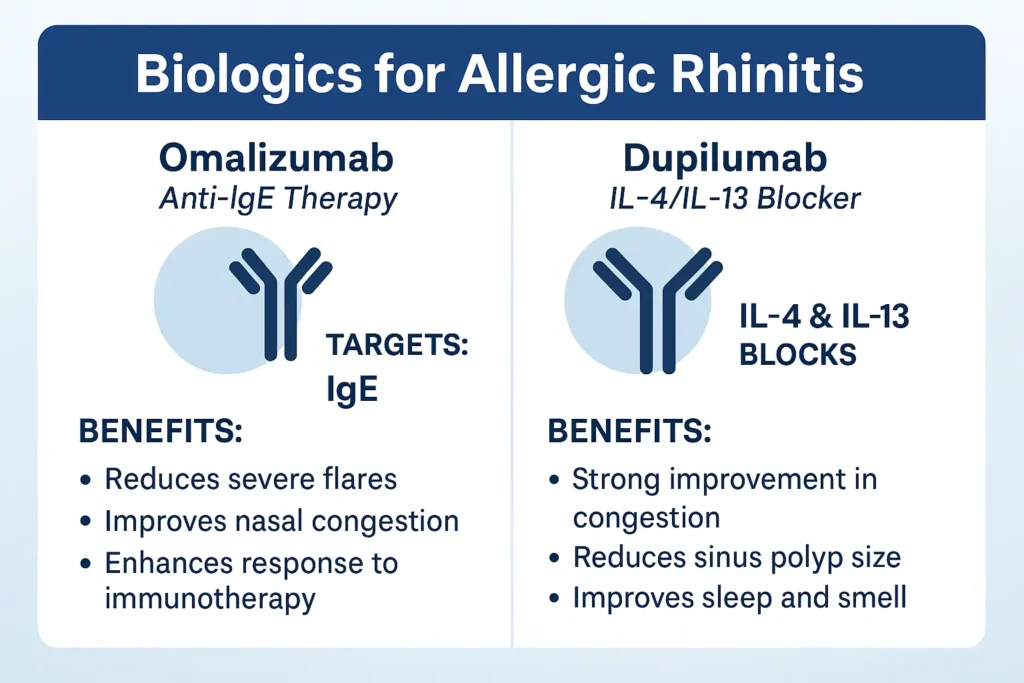
Biologics are advanced injectable medications used for severe allergic disease. They target specific pathways in the immune system.
Biologics for allergic rhinitis comparing anti IgE therapy omalizumab with IL 4 and IL 13 blocker dupilumab
Common biologics include:
- Omalizumab (targets IgE)
- Dupilumab (blocks IL-4/IL-13 inflammation)
Biologics are NOT used for mild rhinitis—only for patients with:
- Severe allergic asthma
- Chronic rhinosinusitis with nasal polyps
- Very severe allergic rhinitis not responding to standard therapy
Evidence shows biologics significantly reduce symptoms, inflammation, and medication use (Klimek et al., 2024).
Omalizumab (Anti-IgE Therapy)
✔ Works Best For:
- Allergic asthma + rhinitis
- High IgE levels
- Indoor allergies (dust mites, pets)
✔ Benefits
- Reduces severe flares
- Improves nasal congestion
- Enhances response to immunotherapy
❌ Limitations
- High cost
- Requires regular injections
- For moderate-to-severe cases only
Dupilumab (IL-4/IL-13 Blocker)
✔ Works Best For:
- Allergic rhinitis with severe asthma
- Nasal polyps
- Chronic sinus inflammation
- Eczema + allergy combination
✔ Benefits
- Strong improvement in congestion
- Reduces sinus polyp size
- Improves sleep and smell
- Reduces steroid dependence
❌ Limitations
- Expensive
- Requires long-term injections
- Possible eye dryness or redness
Children, Pregnancy & Asthma
Children with Allergic Rhinitis
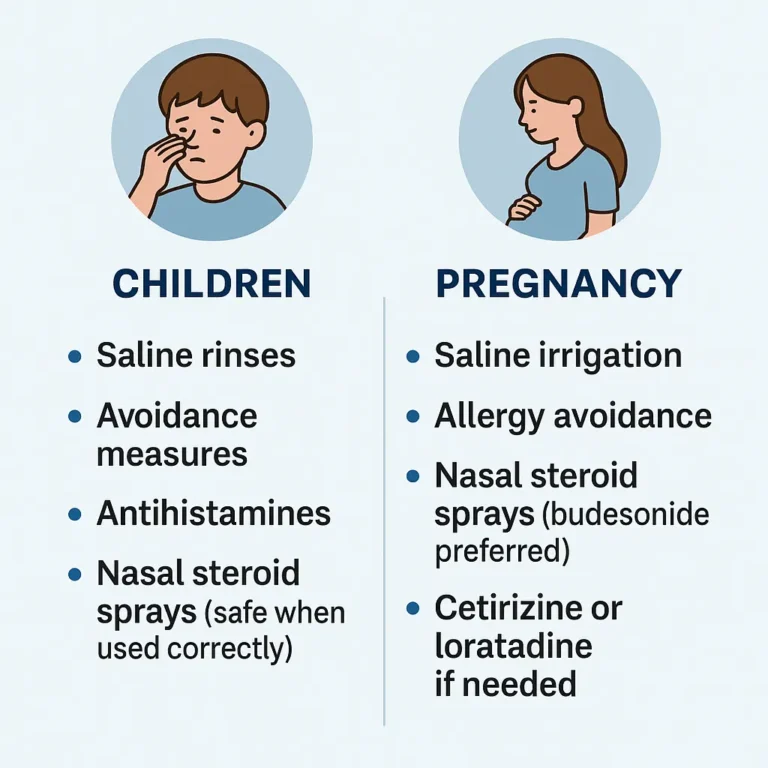
Allergic rhinitis often begins in childhood. Kids respond well to:
- Saline rinses
- Avoidance measures
- Antihistamines
- Nasal steroid sprays (safe when used correctly) (Klimek et al., 2024)
- SLIT (very safe for children)
⚠️ Oral steroids are rarely used in children.
⚠️ Avoid first-generation antihistamines (sedating).
Pregnancy and Breastfeeding
Safest treatments during pregnancy:
- Saline irrigation
- Allergy avoidance
- Nasal steroid sprays (budesonide preferred)
- Cetirizine or loratadine if needed
Systemic steroids should be avoided unless absolutely necessary (Dykewicz et al., 2020).
Asthma + Allergic Rhinitis Overlap
Up to 40–60% of people with allergic rhinitis also have asthma (Bousquet et al., 2020).This interaction is commonly described as allergic rhinitis and asthma overlap.
Rhinitis treatment improves:
- Asthma symptoms
- Lung function
- Nighttime breathing
- Flare frequency
Best treatments for allergy + asthma:
- Nasal steroid sprays
- Oral antihistamines
- Leukotriene receptor antagonists
- Allergen immunotherapy
- Biologics for severe asthma
Difference Between Allergic Rhinitis and Common Cold
Allergic rhinitis is often confused with viral infections. This comparison table helps clarify:
Common Cold vs Allergic Rhinitis
Feature | Common Cold | Allergic Rhinitis |
Cause | Virus | Allergens |
Onset | Slow (1–2 days) | Sudden (minutes to hours) |
Fever | Possible | Never |
Body Aches | Common | Rare |
Nasal Discharge | Thick, colored | Clear, watery |
Sneezing | Mild | Severe, frequent |
Itching | Rare | Very common (eyes, nose) |
Duration | 5–10 days | Weeks–months |
Season | Any time | Pollen seasons or constant (dust mites) |
Response to Antihistamines | Minimal | Strong improvement |
If symptoms last >10 days or recur every year, it is more likely allergic rhinitis, not a cold.
When to See a Specialist
You should see an allergist or ENT if:
- Symptoms persist despite treatment
- You have asthma, eczema, or sinus issues
- You are considering immunotherapy
- You had repeated steroid courses
- You suspect multiple triggers
- You want long-term relief
Key Takeaways
- Oral and injectable steroids work quickly but should be used short-term only.
- Biologics offer powerful relief for severe asthma, rhinitis, and nasal polyps.
- Children and pregnant women need specialized, safer treatment plans.
- Distinguishing between a cold and allergies prevents unnecessary medications.
- Immunotherapy and biologics can provide long-lasting disease modification.
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Are oral steroids safe for allergic rhinitis?
Oral steroids can provide fast relief but should only be used short-term for severe symptoms due to potential side effects.
2. Why are steroid injections not recommended for allergies?
Injectable (depot) steroids stay in the body for weeks and carry higher risks like adrenal suppression and bone loss.
3. Who needs biologic therapy for allergic rhinitis?
Biologics are reserved for severe cases, especially when allergic rhinitis overlaps with asthma or nasal polyps.
4. Can children use steroids or biologics for allergies?
Children usually respond well to nasal sprays and antihistamines; systemic steroids and biologics are rarely needed.
5. How can I tell if I have a cold or allergic rhinitis?
Colds are viral and short-lasting, often with fever, while allergic rhinitis causes itching, clear nasal discharge, and lasts weeks or longer.
6. Is allergic rhinitis linked to asthma?
Yes. Treating allergic rhinitis can improve asthma control, breathing, and reduce flare-ups.
7. When should I see an allergist or ENT specialist?
If symptoms persist, require repeated steroids, involve asthma, or affect daily life, specialist evaluation is recommended.
References
Bousquet, J., Klimek, L., Togias, A., Zuberbier, T., Agache, I., Ansotegui, I. J., … Wallace, D. V. (2020). Next-generation allergic rhinitis and its impact on asthma (ARIA). Journal of Allergy and Clinical Immunology, 145(3), 895–909. https://doi.org/10.1016/j.jaci.2019.12.898
Dykewicz, M. S., Wallace, D. V., Baroody, F., Bernstein, J., Craig, T., Finegold, I., … Portnoy, J. (2020). Rhinitis 2020: A practice parameter update. Journal of Allergy and Clinical Immunology, 146(4), 721–767.
Klimek, L., Bousquet, J., Pfaar, O., Bachert, C., Hellings, P. W., & Agache, I. (2024). Current management of allergic rhinitis: Pharmacologic treatments, non-pharmacologic options and allergen immunotherapy. Journal of Allergy and Clinical Immunology: In Practice, 12(2), 215–229. https://doi.org/10.1016/j.jaip.2023.11.012
Wang, Z., Li, Y., Chen, X., & Zhang, H. (2025). Efficacy and safety of sublingual immunotherapy: An overview of systematic reviews. European Archives of Oto-Rhino-Laryngology, 282(7), 3121–3135. https://doi.org/10.1007/s00405-025-09664-7

