Is Cold Air Bad for Allergic Rhinitis?
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by:Dr Ali Raza Dogar,MBBS,D-LO
Last updated on January 15,2026
Winter Weather, Nasal Congestion, and What Really Happens

Many people with allergic rhinitis (hay fever) notice that their symptoms change during cold weather. Some experience worsening nasal congestion, dryness, sneezing, postnasal drip, or sinus pressure, while others feel temporary relief outdoors but flare up indoors during winter.
This often leads to confusion about whether cold air itself is harmful.
Cold air does not cause allergic rhinitis, but it can irritate inflamed nasal passages and worsen symptoms such as congestion, dryness, postnasal drip, and sinus pressure in people who already have nasal inflammation.
Understanding how cold air affects the nasal lining helps explain winter flare-ups and allows better symptom control.
How Cold Air Affects the Nose and Airways
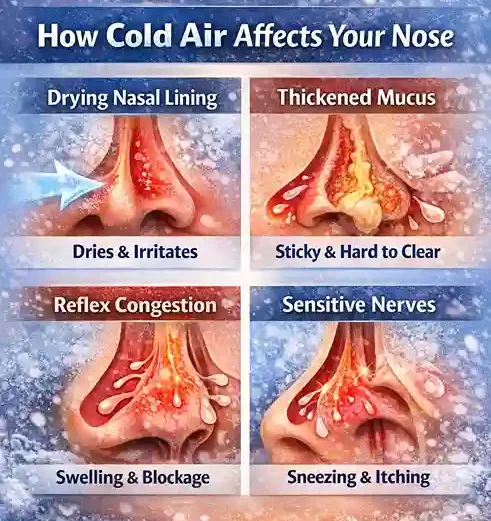
Cold air alters normal nasal function through several physiological mechanisms:
- Low temperatures dry the nasal lining
- Reduced humidity thickens nasal mucus
- Cold triggers reflex swelling of nasal blood vessels
- Sensory nerves become more reactive
For people with allergic rhinitis, whose nasal tissues are already inflamed, these effects are more noticeable. Cold air acts as an irritant, not an allergen, increasing symptoms without triggering an allergic immune response (Eccles, 2002; Dykewicz et al., 2020).
Why Cold Air Can Worsen Allergic Rhinitis Symptoms
1. Drying of the Nasal Mucosa
Cold air contains very little moisture. When inhaled, it dries the nasal mucosa, leading to:
- Nasal dryness and burning
- Thick, sticky mucus
- Reduced natural mucus clearance
- Increased irritation
Dry nasal tissue becomes more reactive, which worsens allergic symptoms during winter (Dykewicz et al., 2020).
Reflex Nasal Congestion (Inferior Turbinates)
Cold exposure triggers a protective reflex in the nose. Blood vessels in the inferior turbinates briefly constrict and then dilate, causing:
- Swelling of nasal tissues
- Increased blockage
- Difficulty breathing through the nose
This reflex nasal congestion can mimic or worsen allergic rhinitis symptoms even without allergen exposure (Bousquet et al., 2020).
Increased Sensitivity of Nasal Nerves
Allergic rhinitis increases sensory nerve sensitivity. Cold air may trigger:
- Sneezing
- Runny nose
- Nasal itching
This reaction is irritation-based rather than allergic, explaining why cold air feels especially aggravating for people with allergies (Eccles, 2002).
Cold Air, Mucus Thickness, and Sinus Pressure
Cold, dry air can:
- Thicken nasal and sinus mucus
- Slow sinus drainage
- Increase facial pressure or headaches
It may also worsen postnasal drip by reducing normal mucus flow. These effects are more noticeable in individuals with allergic rhinitis and sinus sensitivity (Bousquet et al., 2020).
Can Cold Air Ever Help Allergic Rhinitis?
In some cases, cold outdoor air may temporarily reduce symptoms due to lower pollen levels.
Potential benefits include:
- Reduced grass and weed pollen
- Lower outdoor allergen exposure
However, these benefits are often offset by:
- Dry indoor heating
- Increased dust mite exposure
- Mold in poorly ventilated spaces
- Pet dander accumulating indoors
For many people, indoor winter air is a bigger trigger than outdoor cold air (Dykewicz et al., 2020).
Indoor Winter Air: The Hidden Problem
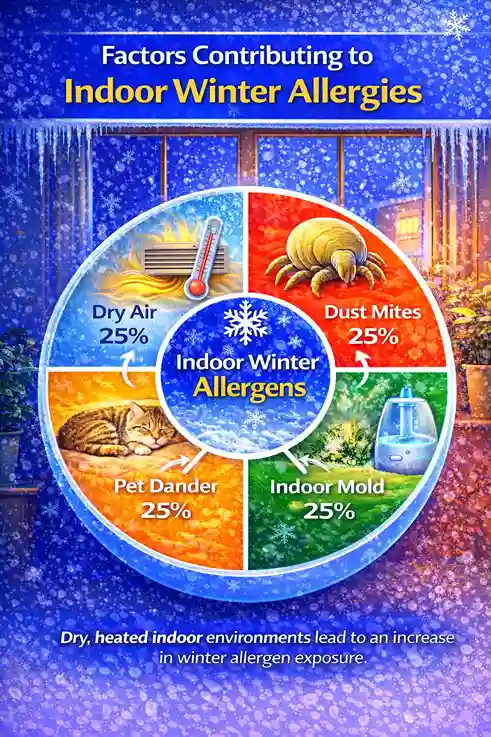
Indoor environments frequently worsen allergic rhinitis during winter.
Common triggers include:
- Dry air from heating systems
- Dust mites in bedding and carpets
- Mold in bathrooms or basements
- Pet dander trapped indoors
Indoor heating often lowers relative humidity below 30%, increasing nasal dryness, irritation, and allergen sensitivity. Managing indoor air quality is essential for winter symptom control (Eccles, 2002).
Cold Air Irritation vs Allergic Rhinitis vs Common Cold
Cold air exposure is often mistaken for illness. Understanding the differences prevents unnecessary treatment.
Feature | Cold Air Irritation | Allergic Rhinitis | Common Cold |
Cause | Temperature & dryness | Allergens | Virus |
Fever | No | No | Common |
Nasal discharge | Clear | Clear | Thick, colored |
Itching | Mild | Common | Rare |
Duration | Short-lived | Persistent | 5–10 days |
Contagious | No | No | Yes |
Cold air does not cause infection but can worsen existing allergic symptoms (Dykewicz et al., 2020).
Cold Air and Nonallergic (Vasomotor) Rhinitis
Cold air can also trigger symptoms in people with nonallergic (vasomotor) rhinitis, a form of noninfectious rhinitis. In this condition, temperature changes—not allergens—cause nasal congestion and runny nose.
This explains why some individuals experience cold-induced nasal symptoms even without allergies.
How to Protect Your Nose in Cold Weather

Warm and Humidify Inhaled Air
- Cover the nose and mouth with a scarf outdoors
- Breathe through the nose when possible
- Avoid sudden temperature changes
Maintain Healthy Indoor Humidity
Aim for 35–50% indoor humidity to:
- Prevent nasal dryness
- Improve mucus clearance
- Reduce dust mite survival
Avoid excessive humidity, which promotes mold.
Support Nasal Moisture
- Saline nasal sprays
- Proper saline irrigation
- Adequate hydration
Moist nasal tissues are less reactive to cold air.
Reduce Indoor Allergens in Winter
- Wash bedding weekly in hot water
- Keep pets out of bedrooms
- Clean dust-collecting surfaces
- Ventilate kitchens and bathrooms
Dress and Exercise Smartly
- Warm up gradually before outdoor activity
- Protect the face and airways
- Choose indoor exercise during extreme cold
Example: Managing Winter Rhinitis with Humidity Control
Some individuals notice improvement after maintaining indoor humidity and using gentle nasal care. Individual responses vary, depending on personal triggers, environment, and overall health.
When to See a Doctor
Consult a healthcare professional if:
- Symptoms persist despite lifestyle measures
- Sinus infections become frequent
- Breathing difficulty or asthma symptoms appear
- Nasal bleeding occurs regularly
Key Takeaways
- Cold air does not cause allergic rhinitis
- It worsens symptoms through dryness and reflex congestion
- Inferior turbinate swelling plays a major role
- Indoor winter air is often more problematic than outdoor cold
- Managing humidity and allergens improves comfort
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Why does my nose block in cold weather?
Cold air causes reflex swelling of nasal blood vessels, leading to congestion.
2. Is cold air an allergen?
No. Cold air is an irritant, not an allergen.
3. Can winter allergies be worse indoors?
Yes. Dust mites, mold, and dry heated air commonly worsen symptoms indoors.
4. Should I avoid going outside in winter?
Not necessarily. Protect your nose and manage indoor air quality.
5. Does cold air cause sinus infections?
Cold air alone does not cause infections, but thickened mucus can increase sinus discomfort.
References
Bousquet, J., Klimek, L., Togias, A., et al. (2020). Next-generation allergic rhinitis and its impact on asthma (ARIA). Journal of Allergy and Clinical Immunology, 145(3), 895–909.
Dykewicz, M. S., Wallace, D. V., Baroody, F., et al. (2020). Rhinitis 2020: A practice parameter update. Journal of Allergy and Clinical Immunology, 146(4), 721–767.
Eccles, R. (2002). Seasonality of upper respiratory symptoms. Acta Oto-Laryngologica, 122(2), 183–191.

