Can Exercise Make Allergic Rhinitis Worse?
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by:Dr Ali Raza Dogar,MBBS,D-LO & Arifa Sarfraz,PT
Last updated on February 21,2026
What Science Says About Physical Activity and Allergy Symptoms
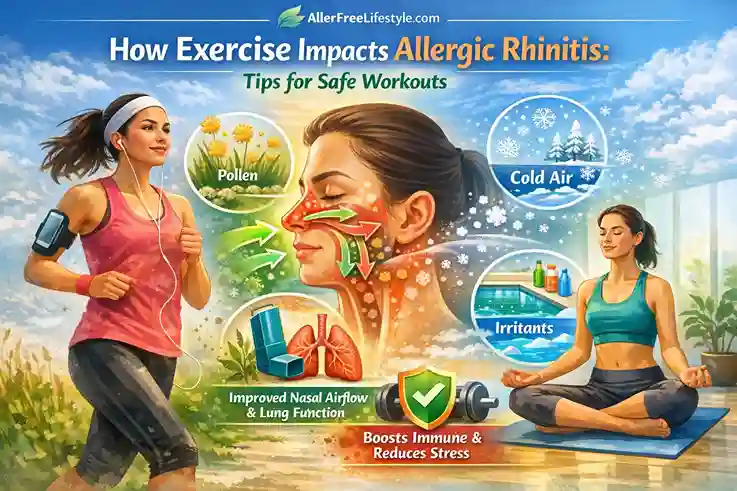
Many people with allergic rhinitis (hay fever) are confused about exercise. Some feel better after physical activity, while others experience worsening sneezing, nasal congestion, or breathing difficulty during or after workouts. This leads to a common and important question:
Can exercise make allergic rhinitis worse?
The short answer is: exercise does not cause allergic rhinitis, but under certain conditions, it can temporarily worsen symptoms. In many cases, the right type of exercise actually improves nasal airflow, lung function, and overall allergy control.
Understanding when and why exercise worsens symptoms—and how to exercise safely with allergies—helps you stay active without triggering flare-ups.
How Exercise Affects Allergic Rhinitis
Exercise influences allergic rhinitis through:
- Breathing patterns
- Airway temperature and humidity
- Exposure to allergens (e.g., pollen)
- Immune and inflammatory responses
The effect can be positive or negative, depending on the situation.
When Exercise Can Make Allergic Rhinitis Worse

1. Outdoor Exercise During High Pollen Levels
Outdoor physical activity during peak pollen seasons is one of the most common triggers for allergic rhinitis.
Why this happens:
- Exercise increases breathing rate
- More pollen enters the nose and airways
- Inflamed nasal tissues react strongly
Exercise and allergic rhinitis are linked because the increased intake of pollen during physical activity worsens symptoms such as sneezing, congestion, and eye irritation. Activities like jogging, cycling, or sports in grassy areas during spring or fall can worsen these symptoms(Bousquet et al., 2020).
To minimize this, consider indoor exercises such as yoga or strength training during peak pollen levels.
2. Cold or Dry Air Exposure
Cold, dry air irritates sensitive nasal passages.
This can lead to:
- Nasal dryness
- Reflex congestion
- Increased sneezing
- Throat irritation
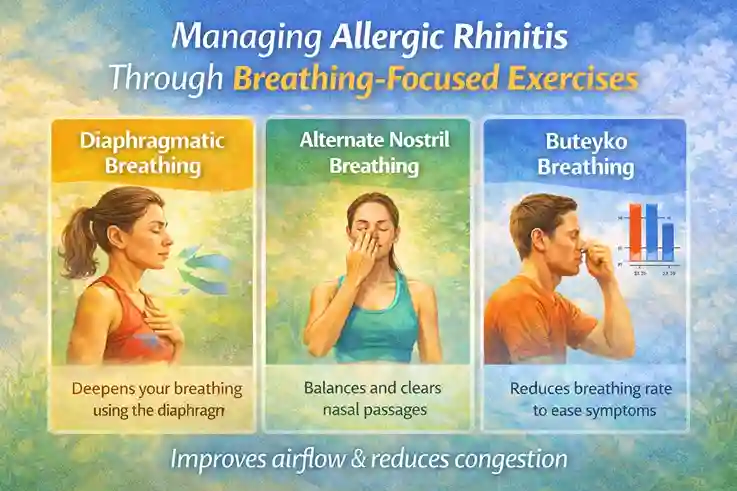
Cold air or dry conditions during winter outdoor exercise or in air-conditioned gyms may worsen symptoms for people with allergic rhinitis. To manage this, consider breathing-focused exercises like diaphragmatic breathing or nasal breathing exercises(Dykewicz et al., 2020).
3. Mouth Breathing During Intense Exercise
During high-intensity workouts, people often breathe through their mouth.
Problem:
- Mouth breathing bypasses nasal filtration
- Allergens, cold air, and pollutants enter directly
This may worsen nasal and throat symptoms after exercise. It’s best to focus on nasal breathing exercises to improve nasal function and prevent further irritation(Carlsen & Carlsen, 2002).
4. Chlorinated Pools and Irritants
Swimming is generally beneficial, but heavily chlorinated pools can irritate nasal mucosa.
Possible effects:
- Burning sensation in the nose
- Nasal congestion
- Sneezing after swimming
This is irritation, not allergy—but it can worsen symptoms in allergic individuals, especially those with exercise-induced rhinitis. To prevent this, choose pools with good air quality and rinse nasal passages afterward(Dykewicz et al., 2020).
5. Exercise-Induced Rhinitis (Non-Allergic Trigger)
Some people experience exercise-induced rhinitis, characterized by a runny nose during physical activity.
This condition:
- Is not caused by allergens
- Occurs due to nerve and blood vessel responses
- Can coexist with allergic rhinitis(Carlsen & Carlsen, 2002)
When Exercise Actually Helps Allergic Rhinitis

Despite the triggers above, regular exercise is beneficial for most people with allergic rhinitis.
Benefits include:
- Improved nasal airflow
- Reduced stress-related inflammation
- Better immune regulation
- Improved lung capacity
- Better sleep quality
Moderate, consistent exercise supports overall respiratory health and helps manage allergic rhinitis symptoms. Even low-intensity outdoor exercises are beneficial when pollen levels are low(Bousquet et al., 2020).
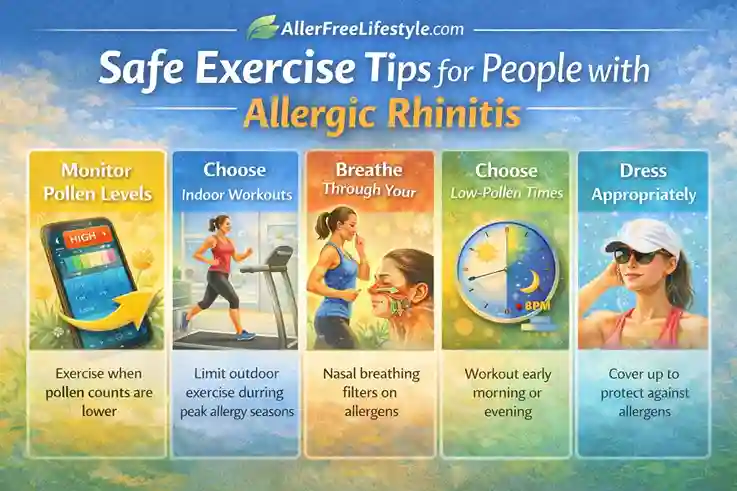
Best Types of Exercise for People With Allergic Rhinitis

1. Indoor Exercise (Best During Allergy Seasons)
Indoor workouts reduce pollen exposure.
Examples:
- Yoga
- Pilates
- Strength training
- Indoor cycling
- Home workouts
Good ventilation and clean indoor air further improve tolerance to exercise, especially during allergy seasons(Dykewicz et al., 2020).
2. Breathing-Focused Exercises
Exercises that emphasize controlled breathing help nasal function and improve airflow.
Examples:
- Diaphragmatic breathing
- Nasal breathing exercises
- Pranayama (gentle forms)
These exercises are beneficial in reducing congestion and improving immune responses to allergens(Carlsen & Carlsen, 2002).
3. Swimming (With Precautions)
Swimming can:
- Improve lung function
- Reduce nasal congestion temporarily
Choose well-maintained pools and rinse nasal passages afterward to minimize irritation(Dykewicz et al., 2020).
4. Low-Intensity Outdoor Exercise (When Pollen Is Low)
If outdoor activity is preferred:
- Exercise early morning after rain or late evening
- Avoid grassy or windy areas
- Wear sunglasses and protective clothing
This reduces exposure to pollen and other allergens, ensuring a safer exercise environment(Bousquet et al., 2020).
How to Exercise Safely With Allergic Rhinitis
Before exercise:
- Check pollen forecasts
- Perform gentle nasal hygiene if needed
- Choose appropriate timing and location
During exercise:
- Warm up gradually
- Breathe through the nose when possible
- Reduce intensity if symptoms appear
After exercise:
- Shower and change clothes
- Rinse nasal passages gently
- Avoid prolonged outdoor allergen exposure(Carlsen & Carlsen, 2002)
Exercise and Allergic Rhinitis With Asthma
Many people have both allergic rhinitis and asthma.
Important points:
- Treating rhinitis improves asthma control
- Warm-up reduces exercise-induced bronchospasm
- Indoor exercise is often safer
Medical guidance is advised if wheezing or chest tightness occurs during exercise(Bousquet et al., 2020).
When to See a Doctor
Consult a healthcare professional if:
- Exercise consistently worsens breathing
- You experience wheezing or chest tightness
- Symptoms persist despite lifestyle adjustments
- Exercise intolerance limits daily activity(Dykewicz et al., 2020)
Key Takeaways
- Exercise does not cause allergic rhinitis but can temporarily worsen symptoms in certain conditions
- High pollen exposure, cold air, and mouth breathing are common triggers
- Regular, well-planned exercise improves overall allergy control
- Indoor and breathing-focused exercises are often best during allergy seasons
- Safe exercise supports immunity, lung health, and quality of life(Carlsen & Carlsen, 2002, Dykewicz et al., 2020)
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Should I stop exercising if I have allergic rhinitis?
No. Most people benefit from exercise when it’s planned properly.
2. Is running bad for allergies?
Running outdoors during high pollen levels can worsen symptoms, but indoor running is usually well tolerated.
3. Can exercise improve nasal congestion?
Yes. Moderate exercise often temporarily improves nasal airflow.
4. Why does my nose run during workouts?
This may be exercise-induced rhinitis, which is not always allergy-related.
5. Is yoga good for allergic rhinitis?
Yes. Yoga and breathing exercises are generally very helpful for nasal breathing and stress reduction【Bousquet et al., 2020】.
References (APA Style)
Bousquet, J., Klimek, L., Togias, A., Zuberbier, T., Agache, I., Ansotegui, I. J., … Wallace, D. V. (2020). Next-generation allergic rhinitis and its impact on asthma (ARIA). Journal of Allergy and Clinical Immunology, 145(3), 895–909. https://doi.org/10.1016/j.jaci.2019.12.898
Dykewicz, M. S., Wallace, D. V., Baroody, F., Bernstein, J., Craig, T., Finegold, I., … Portnoy, J. (2020). Rhinitis 2020: A practice parameter update. Journal of Allergy and Clinical Immunology, 146(4), 721–767.
Carlsen, K. H., & Carlsen, K. C. (2002). Exercise-induced asthma and allergy. European Respiratory Journal, 19(1), 23–31.

