Home, Natural, and Non-Drug Treatments for Allergic Rhinitis (Hay Fever)
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Jamal ud Din Khan, FCPS
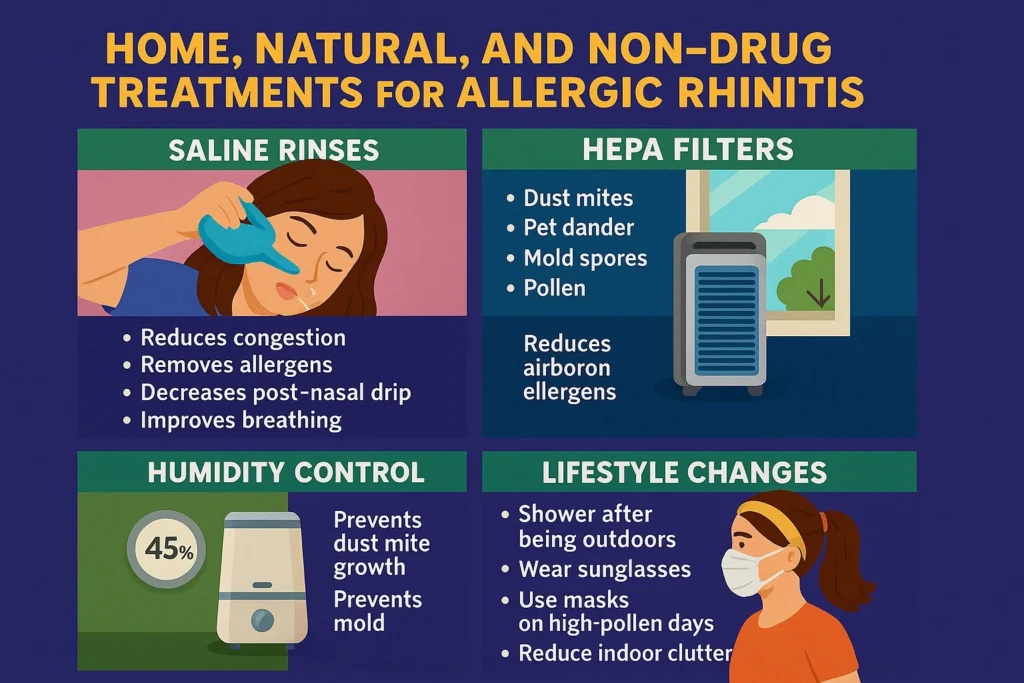
Non-drug treatments are commonly used as supportive strategies in allergic rhinitis management, particularly for individuals seeking to reduce allergen exposure or limit medication use. Evidence shows that measures such as saline irrigation, HEPA filtration, humidity control, and lifestyle modifications can reduce symptom severity when used consistently.
While these methods do not cure allergies, they help remove allergens, reduce inflammation, improve airflow, and support overall nasal health.
Why Natural and Non-Drug Treatments Work
Allergic rhinitis occurs when allergens enter the nose and trigger inflammation. Natural treatments work by:
- Reducing allergen exposure
- Improving nasal hygiene
- Supporting airway function
- Improving indoor air quality
- Enhancing overall breathing comfort
These strategies are strongly recommended in ARIA and AAAAI guidelines (Bousquet et al., 2020).These measures are commonly referred to as natural treatment options for allergic rhinitis in clinical guidelines.
Saline Irrigation & Neti Pot: The Most Effective Natural Remedy
Saline nasal irrigation for allergic rhinitis helps remove allergens, mucus, and inflammatory mediators from the nasal cavity.Patients often ask how to use neti pot for allergic rhinitis. Studies have reported that saline irrigation is one of the most effective natural treatments for allergic rhinitis. It washes out pollen, dust mites, pet dander, mold, mucus, and inflammatory mediators from the nasal cavity (Klimek et al., 2024).
✔Effects of Saline Nasal Irrigation
- Reduces congestion
- Removes allergens
- Decreases post-nasal drip
- Improves breathing
- Enhances the effect of nasal sprays
✔ Forms of Nasal Irrigation
- Neti pot
- Squeeze bottle
- Pressurized nasal rinse
- Saline mist (milder option)
✔ Step-by-Step Safe Use
(ARIA-recommended)
- Always use distilled, boiled, or sterile water (Dykewicz et al., 2020).
- Mix saline powder OR use premixed packets.
- Tilt your head and pour into one nostril, letting it flow out the other.
- Repeat on both sides.
- Clean your device thoroughly after each use.
HEPA Filters and Air Purifiers for Better Indoor Air Quality
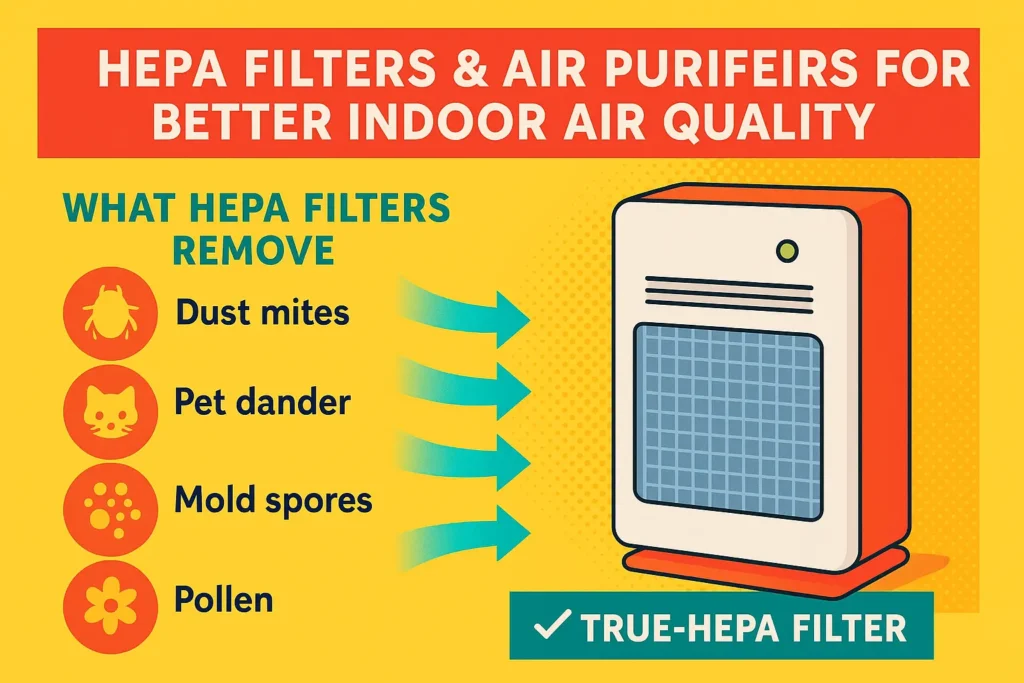
HEPA purifiers show clinically proven benefits for allergic rhinitis and asthma by reducing airborne allergens (Reisman et al., 1990).
✔ What HEPA Filters Remove
- Dust mites
- Pet dander
- Mold spores
- Pollen
- Smoke particles
✔ Placement Matters
- Put one in the bedroom (most important).
- Add another in the living room for added benefit.
✔ Choose a HEPA Filter With:
- High CADR rating
- True-HEPA (not HEPA-like)
- Low noise for nighttime use
Humidity Control: Why Moisture Levels Matter for Allergies

Maintaining indoor humidity between 35–50% helps prevent dust mite growth and mold formation (Klimek et al., 2024).
✔ If humidity is too high:
- Dust mites multiply
- Mold grows
Sinus congestion
✔ If humidity is too low:
- Nose becomes dry
- Irritation worsens
- Nosebleeds may
Proper humidity control for allergic rhinitis helps prevent dust mite growth and mold formation.
Allergen-Proof Bedding to Reduce Dust Mites
Dust mites are the single biggest indoor trigger of perennial allergic rhinitis (Klimek et al., 2024).
✔ Recommended Steps
- Use allergen-proof covers on mattress, pillows, box springs.
- Wash bedding weekly in hot water ≥130°F (54°C).
- Replace heavy carpets with washable rugs.
- Limit stuffed toys or wash them regularly.
Pet Allergy Management in a Natural Way
Pets shed dander (skin protein) that triggers allergic rhinitis.
✔ Natural Strategies
- Keep pets out of the bedroom
- Use HEPA vacuum cleaners
- Wash pets weekly if medically safe
- Use pet allergen-reducing shampoos
Mold Prevention and Removal
Mold spores worsen congestion, sinus presurse, and asthma.
✔ Natural Mold-Control Steps
- Use ventilation in kitchens and bathrooms
- Fix leaks quickly
- Use dehumidifiers
Clean surfaces using anti-mold cleaners
Improving Indoor Air Quality Without Medication

Indoor air quality affects nasal health more than most people realize.
✔ Best Evidence-Based Non-Drug Air Quality Steps
- Use HEPA vacuum cleaners
- Dust using microfiber cloths (captures allergens)
- Avoid incense, strong cleaning chemicals, and aerosols
- Keep windows closed during allergy season
- Maintain good ventilation
These measures represent core non-drug treatment options for allergic rhinitis.
Lifestyle Habits That Reduce Allergic Rhinitis Flares

Small daily changes can noticeably improve symptoms.
✔ Evidence-Based Lifestyle Strategies
- Shower and change clothes after being outdoors (Bousquet et al., 2020)
- Wear sunglasses to reduce pollen entry
- Use masks on high-pollen days
- Reduce indoor clutter (less dust accumulation)
- Avoid cigarette smoke completely
- Exercise indoors when pollen is high
Do Natural Supplements Help Allergic Rhinitis?
Current evidence is limited for many herbal supplements.
However, a few show mild benefit:
✔ Possible but Limited-Benefit Natural Options
- Butterbur (may reduce nasal symptoms)
- Quercetin (anti-inflammatory effects)
- Vitamin C (may reduce histamine slightly)
⚠️ Always consult a doctor before using herbal products.
Evidence remains weaker than medical treatments and environmental controls.
When Natural Treatments Are Not Enough
You should seek medical care if:
- Symptoms persist > 4 weeks
- Congestion is severe
- You have asthma or recurrent sinus infections
- Natural methods help only partially
- You are considering immunotherapy as long-term solution
Key Takeaways
- Natural treatments are powerful and evidence-supported.
- Saline irrigation is the most effective non-drug therapy.
- HEPA filters significantly reduce airborne allergens.
- Humidity control prevents mold and dust mite growth.
- Allergen-proof bedding is essential for dust-mite allergies.
- Lifestyle changes help reduce daily triggers.
- Natural methods work best when combined with proper medical treatment.
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
1. Do natural treatments really help allergic rhinitis?
Yes. Saline rinses, HEPA filters, humidity control, and allergen reduction have strong clinical evidence for reducing symptoms and improving nasal comfort.
2. How often should I use saline nasal irrigation?
Most people benefit from using saline rinses once daily, or twice daily during high allergy seasons or severe symptoms.
3. Are HEPA air purifiers effective for allergies?
Yes. True HEPA filters significantly reduce airborne allergens like pollen, dust mites, pet dander, and mold spores, especially in bedrooms.
4. What indoor humidity level is best for allergy prevention?
An indoor humidity range of 35–50% helps prevent dust mite growth and mold while keeping nasal passages comfortable.
5. Can allergen-proof bedding really reduce symptoms?
Yes. Using dust-mite-proof mattress and pillow covers and washing bedding weekly in hot water can greatly reduce perennial allergy symptoms.
6. Are natural supplements enough to control allergic rhinitis?
Usually not. Supplements may offer mild benefit, but environmental control and nasal hygiene are far more effective and evidence-based.
7. When should I see a doctor despite using natural methods?
If symptoms last longer than 4 weeks, are severe, or occur with asthma or sinus infections, medical evaluation is recommended.
REFERENCES
Bousquet, J., Klimek, L., Togias, A., Zuberbier, T., Agache, I., Ansotegui, I. J., … Wallace, D. V. (2020). Next-generation allergic rhinitis and its impact on asthma (ARIA) guidelines. Journal of Allergy and Clinical Immunology, 145(3), 895–909. https://doi.org/10.1016/j.jaci.2019.12.898
Dykewicz, M. S., Wallace, D. V., Baroody, F., Bernstein, J., Craig, T., Finegold, I., … Portnoy, J. (2020). Rhinitis 2020: A practice parameter update. Journal of Allergy and Clinical Immunology, 146(4), 721–767.
Klimek, L., Bousquet, J., Pfaar, O., Bachert, C., Hellings, P. W., & Agache, I. (2024). Current management of allergic rhinitis: Pharmacologic and non-pharmacologic options. Journal of Allergy and Clinical Immunology: In Practice, 12(2), 215–229. https://doi.org/10.1016/j.jaip.2023.11.012
Reisman, R. E., Mauriello, P. M., Davis, G. B., Georgitis, J. W., & DeMasi, J. M. (1990). Effectiveness of HEPA filters in allergic rhinitis and asthma. Journal of Allergy and Clinical Immunology, 85(6), 1050–1057.

