Immunity, Nutrition & Anti-Inflammatory Diet for Allergic Rhinitis
Written by: Dr.Muhammad Ihsan Ullah, PhD
Medically reviewed by: Dr. Jamal Ud Din Khan,FCPS
Last updated on February 04, 2026
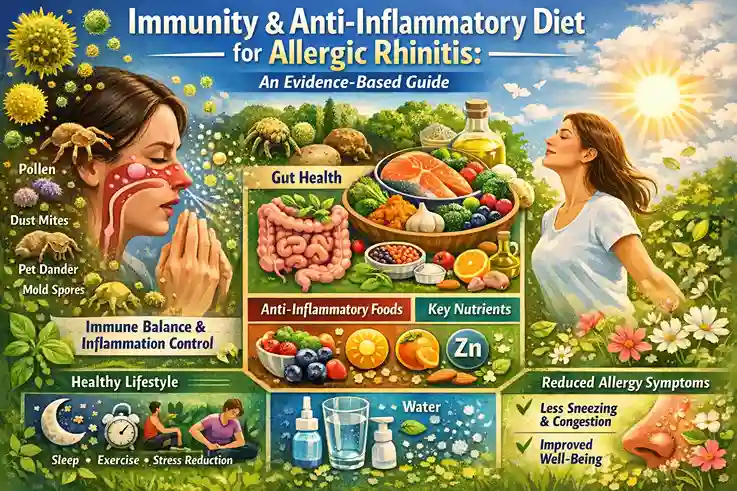
Allergic rhinitis (hay fever) is not caused by a weak immune system—it is caused by an overreactive and dysregulated immune response to harmless airborne allergens such as pollen, dust mites, pet dander, and mold spores.
For this reason, the goal is not to “boost” immunity, but to support immune balance, reduce inflammation, and improve barrier defense of the nasal and respiratory system.
Research shows that nutrition, gut health, micronutrients, hydration, and anti-inflammatory dietary patterns play a meaningful role in reducing allergy symptom severity, flare frequency, and overall disease burden—especially when combined with standard medical care (Bousquet et al., 2020; Klimek et al., 2024).
Understanding Immunity in Allergic Rhinitis

In allergic rhinitis:
- The immune system produces IgE antibodies
- Mast cells release histamine and inflammatory mediators
- Nasal tissues become swollen, itchy, and congested
This process reflects immune hypersensitivity, not immune deficiency.
Therefore, lifestyle strategies focus on:
- Reducing chronic inflammation
- Supporting mucosal barrier integrity
- Modulating immune signaling
Improving gut–immune interaction
The Gut–Immune–Allergy Connection
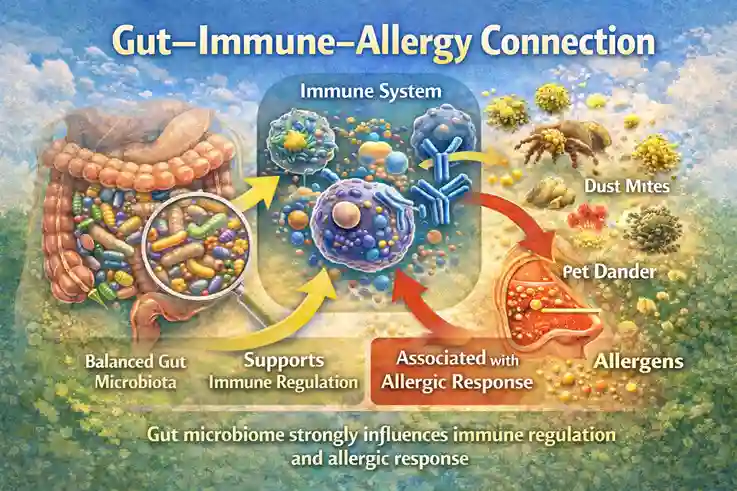
More than 70% of immune cells reside in the gut, and gut microbiota strongly influence immune tolerance.
Studies show:
- Gut dysbiosis is associated with allergic diseases
- Balanced gut microbiota supports immune regulation
- Diet directly shapes immune response patterns
Supporting gut health is a core pillar of allergy-friendly living (Noverr & Huffnagle, 2004).
Anti-Inflammatory Diet Pattern for Allergic Rhinitis
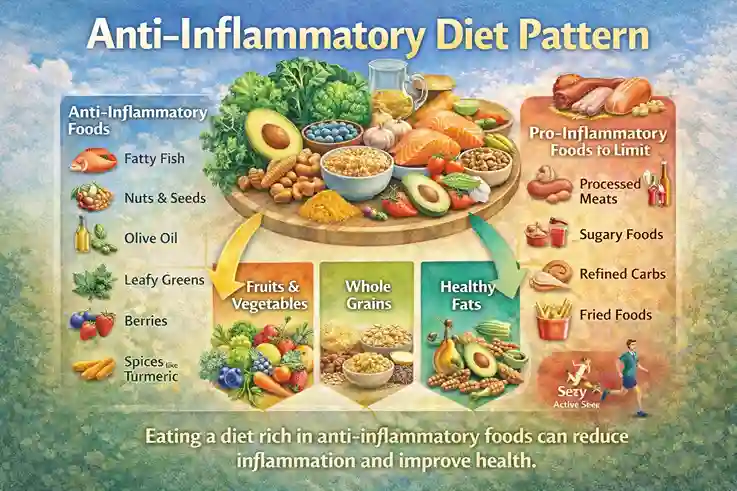
Rather than focusing on single “superfoods,” evidence supports dietary patterns that reduce systemic inflammation.
Core Principles
- Whole, minimally processed foods
- High antioxidant intake
- Adequate omega-3 fatty acids
- Reduced ultra-processed foods
Stable blood sugar levels
Foods That Support Immune Balance & Allergy Control

Omega-3 Fatty Acid–Rich Foods
Examples:
- Fatty fish (salmon, sardines)
- Flaxseeds
- Chia seeds
- Walnuts
Why they help:
Omega-3 fatty acids reduce inflammatory mediator production and may counterbalance allergic inflammation (Calder, 2017).
Antioxidant-Rich Fruits & Vegetables
Examples:
- Berries
- Citrus fruits
- Spinach
- Broccoli
- Bell peppers
Benefits:
- Neutralize oxidative stress
- Support nasal mucosal integrity
- Reduce inflammatory burden
Foods Supporting Gut Microbiota
Examples:
- Yogurt with live cultures
- Kefir
- Fermented vegetables
- Fiber-rich foods (oats, legumes)
Healthy gut flora supports immune tolerance and reduces allergic sensitization.
Natural Anti-Inflammatory Foods
Examples:
- Turmeric
- Ginger
- Garlic
- Green tea
These contain bioactive compounds that modulate inflammatory pathways.
Micronutrients Important for Allergic Rhinitis

Vitamin D
Low vitamin D levels are associated with increased allergic rhinitis severity.
Sources:
- Sunlight
- Fortified foods
- Supplements (if deficient)
Vitamin D supports immune regulation rather than immune stimulation (Wang et al., 2019).
Vitamin C
Acts as a mild natural antihistamine and antioxidant.
Sources:
- Citrus fruits
- Kiwi
- Strawberries
- Bell peppers
Zinc
Supports epithelial barrier integrity and immune signaling.
Sources:
- Nuts
- Seeds
- Whole grains
- Meat and legumes
Hydration & Nasal Mucosal Health
Adequate hydration:
- Keeps nasal mucus thin
- Improves sinus drainage
- Reduces irritation
Tip:
Aim for consistent fluid intake throughout the day rather than large volumes at once.
Foods & Habits That May Worsen Allergy Symptoms
Some people report symptom worsening with:
- Highly processed foods
- Excess sugar
- Alcohol
- Artificial additives
- Very spicy foods (in sensitive individuals)
Triggers vary individually; symptom journaling helps identify patterns.
Role of Natural Supplements
Some supplements show modest benefit, but none replace medical therapy.
Supplements with limited evidence:
- Quercetin
- Butterbur (PA-free only)
- Probiotics (strain-specific)
⚠️ Always consult a healthcare provider before using supplements, especially with medications.
Lifestyle Factors That Support Immune Balance
Nutrition works best when combined with:
- Consistent sleep (7–9 hours)
- Stress reduction
- Gentle physical activity
- Breathing exercises
- Environmental allergen control
These factors reduce inflammatory load and improve immune resilience.
What Nutrition Can and Cannot Do
✔ Can:
- Reduce symptom severity
- Support immune regulation
- Improve nasal comfort
- Enhance overall health
❌ Cannot:
- Cure allergic rhinitis
- Replace prescribed medication
- Eliminate severe allergies alone
Balanced nutrition is supportive, not curative.
When to Seek Medical Guidance
Consult a healthcare professional if:
- Symptoms persist despite lifestyle changes
- Asthma symptoms occur
- Frequent sinus infections develop
- Considering supplements or elimination diets
Medical Review Disclaimer
This article is for informational and educational purposes only and does not constitute medical advice. The content is written by a qualified healthcare professional and medically reviewed for accuracy. However, it should not be used as a substitute for professional medical diagnosis, treatment, or advice. Always consult a licensed healthcare provider regarding any medical condition or health concern.
Frequently Asked Questions (FAQs)
Does improving immunity cure allergic rhinitis?
No. Allergic rhinitis involves immune overreaction, not immune weakness
Can diet really affect allergy symptoms?
Yes. Anti-inflammatory dietary patterns reduce symptom burden.
Are supplements better than food?
Whole foods provide broader benefits; supplements are secondary.
Is this approach safe for children and elderly?
Yes, when based on balanced nutrition and not restrictive diets.
References
Bousquet, J., Klimek, L., Togias, A., Zuberbier, T., Agache, I., Ansotegui, I. J., … Wallace, D. V. (2020). Next-generation allergic rhinitis and its impact on asthma (ARIA). Journal of Allergy and Clinical Immunology, 145(3), 895–909. https://doi.org/10.1016/j.jaci.2019.12.898
Calder, P. C. (2017). Omega-3 fatty acids and inflammatory processes. Nutrients, 9(9), 989. https://doi.org/10.3390/nu9090989
Klimek, L., Bousquet, J., Pfaar, O., Bachert, C., Hellings, P. W., & Agache, I. (2024). Current management of allergic rhinitis: Pharmacologic and non-pharmacologic options. Journal of Allergy and Clinical Immunology: In Practice, 12(2), 215–229. https://doi.org/10.1016/j.jaip.2023.11.012
Noverr, M. C., & Huffnagle, G. B. (2004). Does the microbiota regulate immune responses outside the gut? Trends in Microbiology, 12(12), 562–568. https://doi.org/10.1016/j.tim.2004.10.008
Wang, Y., Li, J., Guo, S., & Zhao, L. (2019). Vitamin D deficiency and allergic rhinitis. American Journal of Rhinology & Allergy, 33(3), 308–314. https://doi.org/10.1177/1945892419826971

